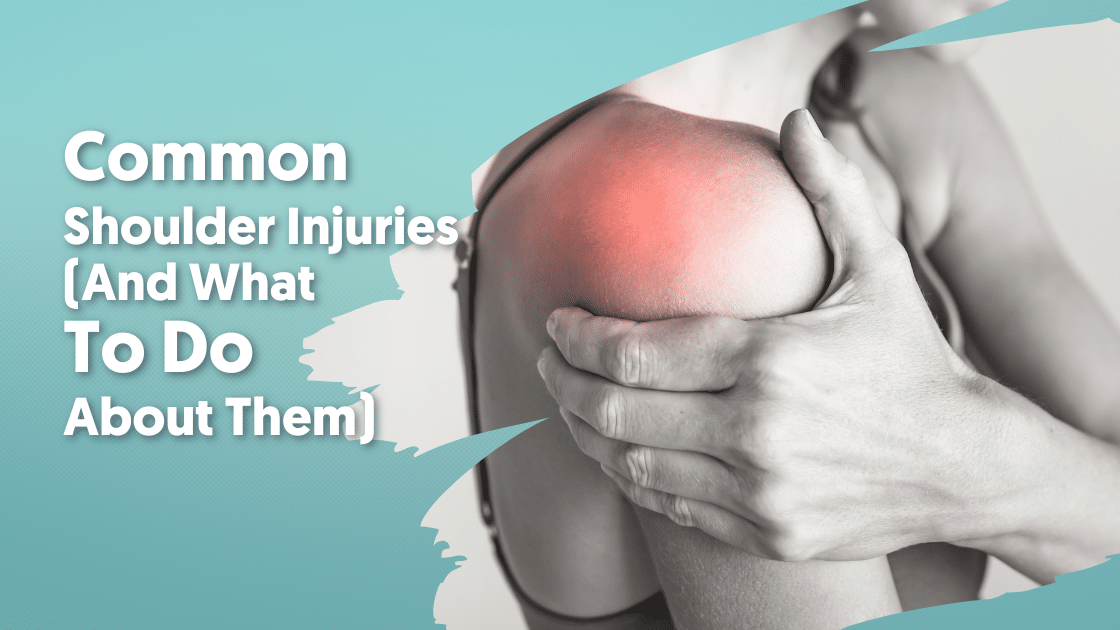
Shoulder injuries are far from uncommon. After all, shoulders are the most movable joints in your body. They have to be anchored down just to stay in a normal, stable position. And since they can become unstable so easily, it’s no wonder there’s so many shoulder injuries.
Your shoulder is made up of 2 main joints, along with muscles, tendons, ligaments, cartilage, bones, and a bursa. This article will attempt to discuss the most common shoulder injuries related to these structures and what you can do about them.
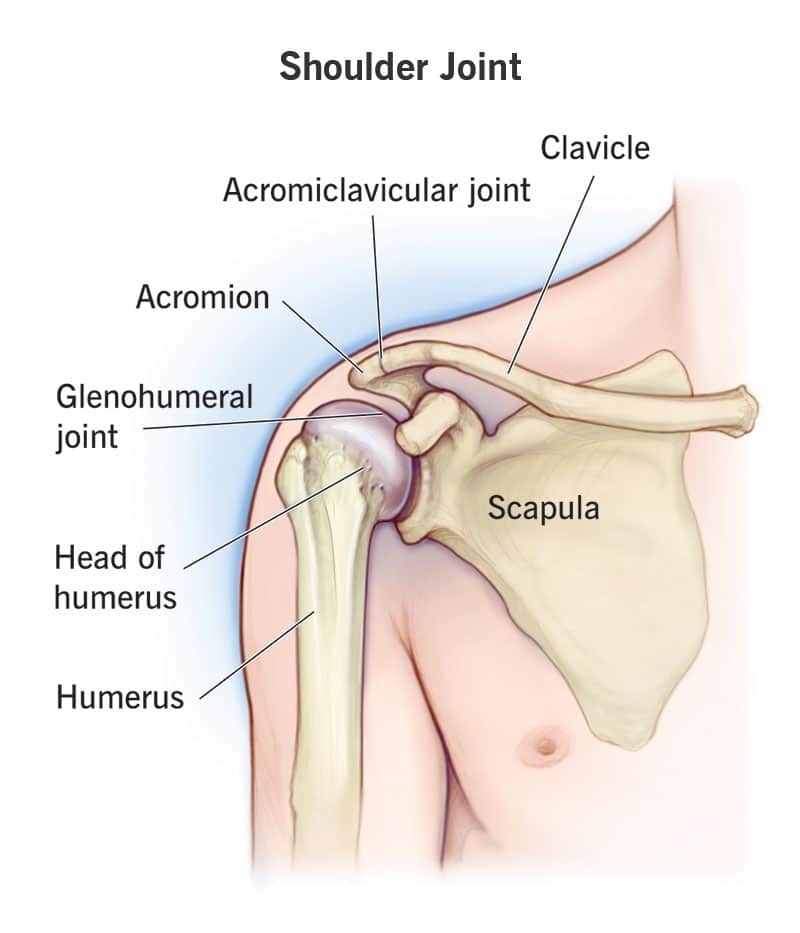
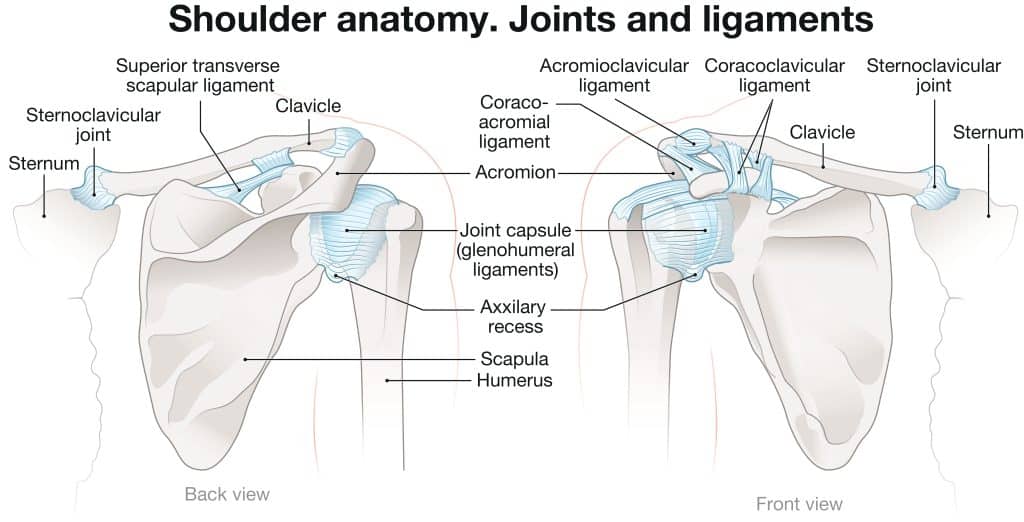
First, let’s take a look at some basic anatomy. There are 3 bones that form your shoulder: the collarbone or clavicle, the shoulder blade or scapula, and the upper arm bone or humerus.
The area where your bones meet and allow for movement is called a joint. You have 2 joints that join your shoulder bones together, the acromioclavicular joint and the glenohumeral joint. The acromioclavicular joint connects the top of your shoulder blade (acromion) and your collarbone (clavicle). Hence the name, acromioclavicular. It kind of resembles two pencils lined up together with a small gap in the middle. Your glenohumeral joint is a ball and socket type joint that connects your upper arm bone (humerus) into your shoulder blade (glenoid cavity). The “ball” portion of the ball and socket is actually bigger than the socket that holds it, which is a big reason why your shoulder is naturally so unstable.
Cartilage
Cartilage is thin flexible tissue that covers every part of a bone that touches another bone. It’s on the ends of your collarbone, shoulder blade and upper arm bone. Cartilage helps your shoulder glide smoothly when you move and it protects your bones so you don’t experience any pain, grinding, or clicking.
Ligaments & Tendons
Ligaments are the things that connect bones to other bones. They keep your skeleton together and give it structure. As for tendons, they’re just bundles of fibers that connect your muscles to your bones. Both of these help support and hold your shoulder joint together.
Bursa
Last but not least is your bursa. A bursa is a sac of fluid that cushions the space between everything in your joint. You have your bursa to thank for your tendons, ligaments, and muscles being able to move freely.
So, now that you’ve had a brief overview of everything that makes up your shoulder, let’s take a closer look at muscles and tendons.
Muscle & Tendon Injuries
There are several muscles in your shoulder, 4 of which come together as tendons and cover the head of your humerus. They’re known as your rotator cuff and they work together to stabilize your shoulder joint. They’re also the reason you’re able to lift, reach, and rotate your arm.
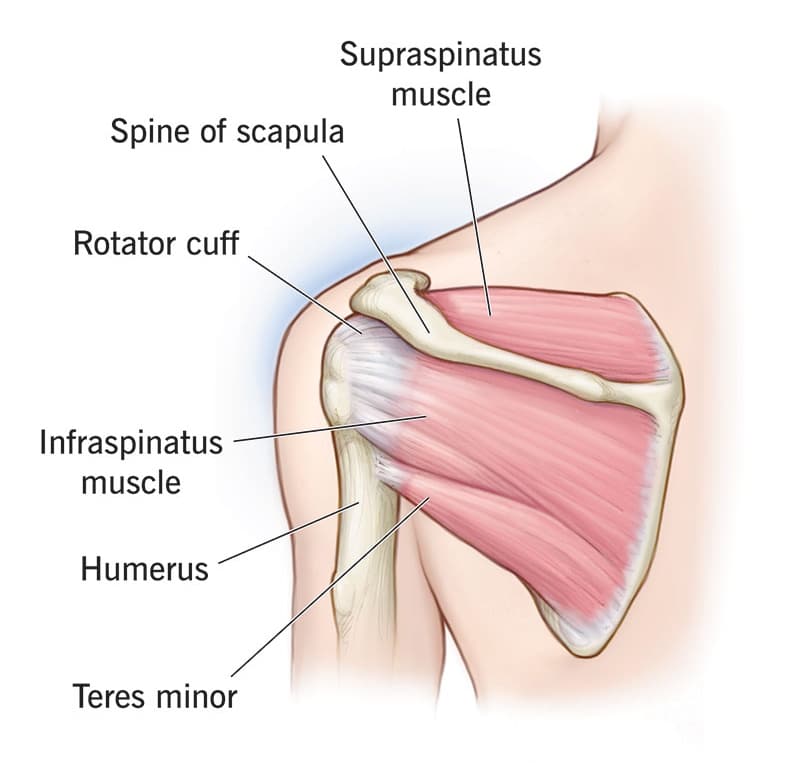
As you can see, your shoulder joint is supported on all sides by your muscles and tendons. Of course, they can only take so much force before they rub, stretch, and occasionally even tear. Now it’s time to go over some muscle and tendon injuries.
Rotator Cuff Tears
One of the most common and widely known shoulder injury is a torn rotator cuff. It’s so common in fact, that nearly 2 million people experience one every year. Your rotator cuff is made up of 4 muscles: subscapularis, supraspinatus, infraspinatus, and teres minor. The ends of these muscles form tendons, attaching your upper arm bone to your shoulder blade.
It’s because of your rotator cuff that you’re able to move your arm in so many different ways. Each muscle plays a different role. The subscapularis muscle is responsible for internally rotating your arm. Supraspinatus is what lets you lift and hold your arm away from your body. Both the infraspinatus and teres minor muscles rotate your arm externally.
When you have a rotator cuff tear, it can be either a partial tear or a full thickness tear. As their names suggest, partial tears don’t completely rip from the bone (only partially), whereas full thickness tears are fully detached.
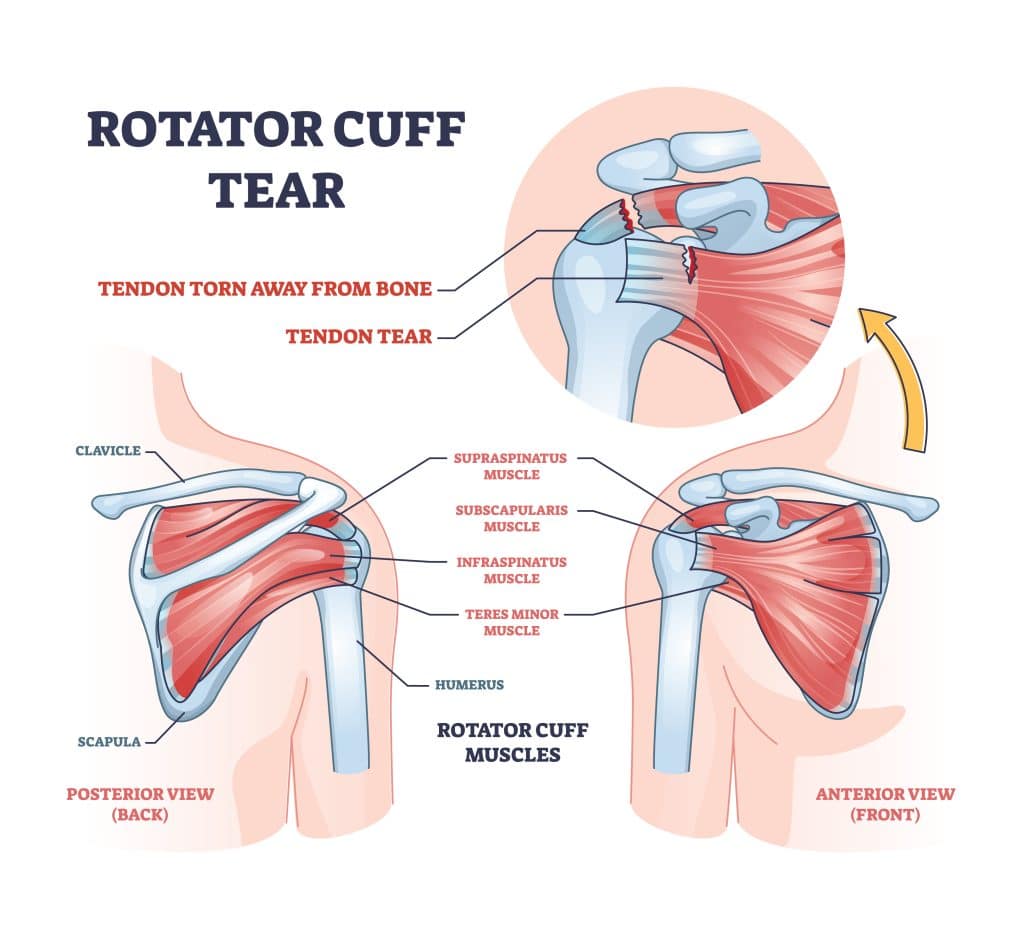
Typically, the tendon that gets torn the most is supraspinatus, but the other 3 can also be involved. They usually start out by fraying and as the damage progresses, it turns into a complete tear, often after lifting something really heavy.
Symptoms:
When you tear your rotator cuff, you’ll notice a few things. The first is pain, regardless if you’re resting your arm or moving it. You might also feel weakness when you’re lifting or a crackling popping sensation known as crepitus.
Tears that develop gradually are usually a result of overuse. At first, you might not have any symptoms. Then, you’ll get some mild pain when you reach overhead or lift your arm. After a while, the pain becomes more apparent, especially when you’re resting. You’ll probably start noticing trouble doing daily tasks too, like combing your hair or pulling a belt through the back loops of your pants.
Tears that happen suddenly though, like from a fall, can feel like a snapping sensation followed by intense pain. You’ll also notice your arm immediately feeling weak afterwards.
Causes:
There’s 2 main things that can cause rotator cuff tears: injury and degeneration.
Injury related tears are actually fairly common. It can be as simple as bracing your arm while you’re falling or even a quick jerking movement while lifting something heavy. There’s usually some other injuries that happen along with the tear too, like breaking your wrist or dislocating your shoulder.
Most rotator cuff tears happen, though, after the tendon wears down slowly over time. Degeneration like this is just part of the natural aging process and is relatively painless in most cases. You’ll most likely tear a tendon in your dominant arm since it’s the one you use the most. And once you get a tear in one of your shoulders, there’s a higher chance of developing a tear in the other shoulder too, even if you don’t notice any pain.
Several things can play a part in wear-and-tear type rotator cuff tears. Possibly the biggest contributing factor is repetitive stress. By doing the same movements over and over again, you’re continuously stressing and straining your rotator cuff muscles and tendons. Anything from work related tasks to routine chores, and even certain sports with repetitive lifting or overhead movements can put your shoulder at risk for overuse tears.
Diagnosing:
After discussing your symptoms and medical history, your doctor will examine your shoulder for a rotator cuff tear. The exam will test your range of motion, assess your arm strength, and look for any other injuries you may have. They might even examine your neck to rule out things like arthritis or a pinched nerve.
Your doctor could decide to order x-rays to check out the bones in your shoulder joint. Since x-rays don’t show soft tissue like your rotator cuff muscles or tendons, they can sometimes look normal even when there’s a tear. Occasionally, an x-ray might reveal an old, degenerative tear that was never diagnosed because it wasn’t causing you any symptoms.
You might also be sent to get an MRI, which are great for soft tissue injuries like rotator cuff tears. They can determine the size and location of your tear. Plus, they can also indicate whether your tear is recent or not by showing the condition of your rotator cuff muscles.
Treatment:
It’s definitely not a good idea to push through the pain of a torn rotator cuff. Your tear can grow over time and cause even more problems down the road. So, if your shoulder is constantly aching, go see your doctor.
Treatment will depend on your age, overall health, activity level, and the type of tear you have, but most people have great success without needing surgery.
One of the safest and most effective treatment options is actually physical therapy. The goal with all rotator cuff tears is to strengthen the muscles around your shoulder joint. This lowers your risk of reinjury and also helps ease your pain too.
Your therapist will create a customized exercise program that focuses on improving your flexibility and range of motion. They’ll also help make modifications to any of your daily tasks or activities that could strain your shoulder and make your injury worse. As you progress, your exercise program and modifications will be adjusted too.
Some people choose to get cortisone steroid injections to help with their pain. While cortisone can be an effective anti-inflammatory, it doesn’t always work for everyone. There’s also no way to tell how long the effects of the shots will last. Not to mention, these shots are only masking your symptoms. In order to find true relief, you need safe, guided movement from a physical therapist or your problem is going to keep coming back.
Rotator Cuff Impingement
The term “impingement” simply refers to rubbing or pinching inside of your joint. Rotator cuff impingement, or shoulder impingement syndrome, is when the outer edge of your shoulder blade is pinching your rotator cuff and the bursa underneath your acromion. This causes swelling and inflammation, which can be pretty painful, especially when you raise your arm away from your body.
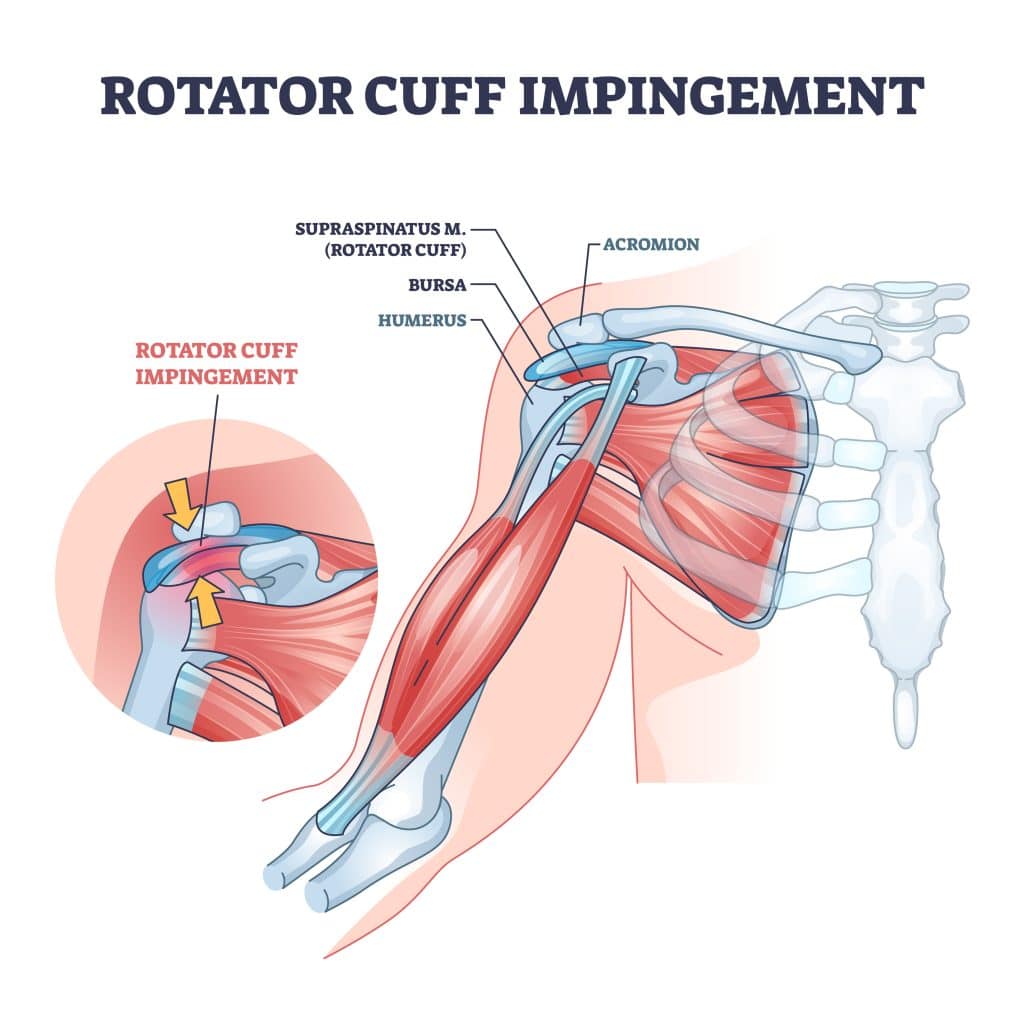
Rotator cuff impingement is classified by 3 grades. Grade 1 impingement involves inflammation in your tendons and bursa. Moving to grade 2 means there’s scarring and thickening of your bursa. You’ve made it to grade 3 when you have degeneration and tears in your rotator cuff tendons.
You can get impingement in other parts of your body, but shoulders are the most common. More than 50% of all shoulder pain cases are from rotator cuff impingement. It’s especially true for athletes and anyone with a physically demanding job.
Symptoms:
One of the most common symptoms of rotator cuff impingement is having pain in the front of your shoulder. It might feel tender to the touch, radiate down the side of your arm, or get worse as your day goes on.
Certain positions can increase your pain. Some of these movements include:
- Extending your arm above your head
- Raising and lowering your arm
- Reaching out for something
- Laying on your injured arm
- Reaching behind your back
You might experience some other symptoms too, like stiffness or a popping cracking sound when you move.
Causes:
Rotator cuff impingement is almost always caused by overuse. It happens over time when you repeat a motion or activity that puts too much stress on your shoulder and rotator cuff. For most people, it develops slowly, over the course of several weeks or months.
Typically, it’s overhead rotation that leads to impingement. So, basically any motion where you have to twist and turn with your arms raised up. This is an issue for anyone that has to do these same movements at work every day, like construction workers or window washers. Trauma, like a fall or car accident, can also cause impingement as well.
Diagnosing:
A doctor can diagnose your impingement through a simple exam. They’ll move your shoulder in different directions to see how far it goes without causing pain. You’ll want to tell them what you were doing when you first noticed the pain, and if any of your hobbies or work involve repetitive arm movements.
There’s a chance your doctor could order x-rays or an MRI to help determine the cause of your impingement. The imaging will also rule out any other issues that might be causing you pain, like arthritis or a torn tendon.
Treatment:
Taking pain meds or getting steroid shots might take the edge off at first, but they’re just a bandaid. What’s going to help with rotator cuff impingement the most is movement, and that’s where physical therapy really shines.
At physical therapy, you’ll learn the tools to manage your symptoms and help your shoulder heal while regaining your function at the same time. The PT will work with you to improve your strength and range of motion through stretches and exercises. As you progress through your plan of care, they will add to your exercise list so you can continue strengthening your rotator cuff muscles.
Most people with rotator cuff impingement start feeling better within the first few weeks of starting PT. You’ll be able to slowly get back to your normal activities, maybe with a few modifications in the beginning, but you won’t need them forever.
Biceps Tendinitis
Biceps tendinitis is exactly what it sounds like, tendinitis in your biceps. The “itis” part of tendinitis refers to inflammation, so in this case, it’s inflammation of your biceps tendon. You can get biceps tendinitis (sometimes written as tendonitis) when your upper biceps tendon gets irritated and becomes inflamed. The tendon in question, called the long head of the biceps tendon, connects your biceps muscle to your shoulder blade.
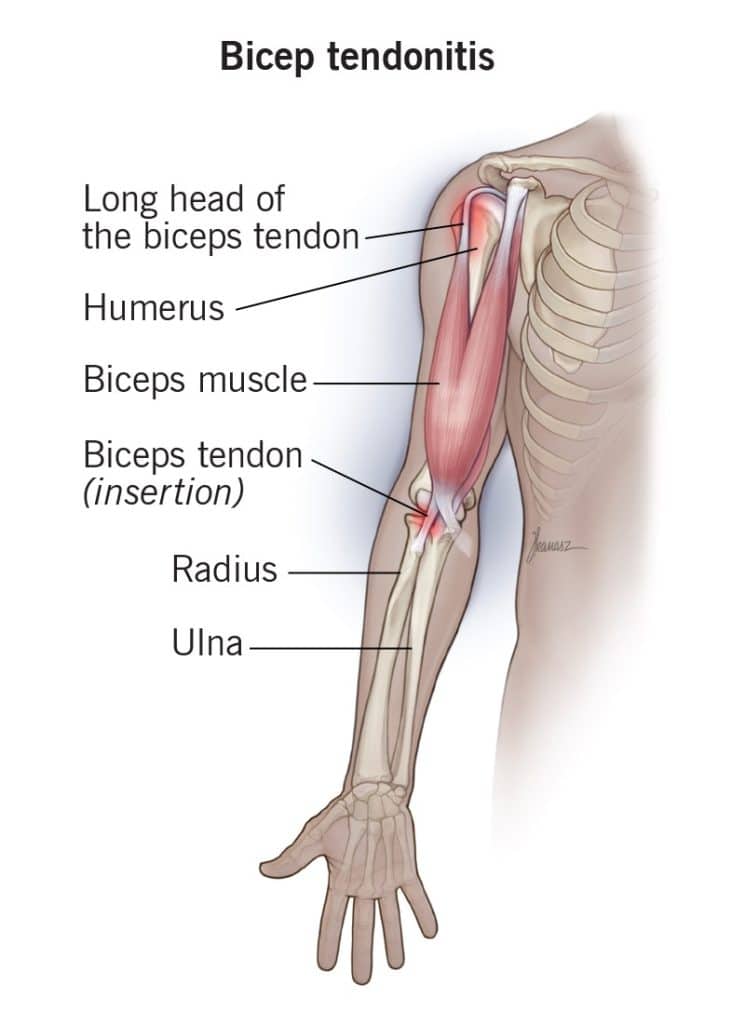
This type of tendinitis is usually caused by overuse, especially from repetitive overhead movements, or if there’s a sudden heavy strain on your tendon. There’s typically other conditions that develop alongside the tendinitis, like arthritis or a dislocated shoulder.
Symptoms:
With biceps tendinitis, you’ll have pain and tenderness in the front of your shoulder. You’ll notice it getting worse if you’re exercising or raising your arm up, and you might even feel pain running down your arm or hear a snapping sound in your shoulder.
Causes:
Biceps tendinitis usually develops slowly over time just from everyday wear and tear on your tendons. Your tendons naturally get weaker as you age, so overusing them can make things worse. When you do the same motions over and over, day in and day out, it’s that repeated wear and tear on your shoulder that leads to this condition.
It’s not just tendinitis that you have to worry about either. If you’re in a situation where you’re constantly overusing your biceps, you also run the risk of eventually tearing the tendon. You can get a tear from an injury too, like twisting your shoulder the wrong way or falling with your arm stretched out.
Tears can be classified as either partial or complete. If you have a partial tear, some of the tendon is still attached to the bone. A complete tear, also called a biceps tendon rupture, means your tendon has fully torn away from the bone.
There are 2 tendons that attach your biceps muscle to your shoulder, but only one, the distal biceps tendon, attaches to your elbow. It’s pretty rare to tear this tendon, but when it happens, it’s usually because of an injury or from lifting something heavy. It’s almost always a complete tear too, which can make certain movements, like twisting a screw driver, much weaker than normal.
Diagnosing:
To diagnose biceps tendinitis, your doctor is going to check how well your biceps is working. This includes testing strength, stability, and range of motion.
They may also request imaging as well. X-rays will show if there’s any other problems in your shoulder joint, while an MRI will let them know whether your tendon is torn, how irritated it is, and if there’s any inflammation.
Treatment:
Treating biceps tendinitis typically starts with physical therapy. It’s important that you avoid things that can make your condition worse, like heavy lifting or reaching overhead, so you’ll need to learn what movements are safe to do, especially while you’re just starting to heal.
At PT, your therapist will teach you exercises and stretches that strengthen your shoulder and restore your range of motion. Balancing out your muscles is what’s going to keep your shoulder joint protected and moving smoothly.
Physical therapists are trained to do hands-on therapy techniques, which means they can target areas of your body that you aren’t able to reach yourself. They’ll be able to move your shoulder joint and the muscles around it to help with your motion and flexibility.
Your recovery will depend on the severity of your tendinitis, but you should notice improvement pretty quickly.
Ligament Injuries
One of the most important structures in your shoulders are your ligaments. Ligaments connect bones to other bones and form a capsule around your joint. While they’re fairly shorter compared to tendons, ligaments are your main source of stability (which is why they’re so important since your shoulder is so unstable.)
Adhesive Capsulitis (Frozen Shoulder)
A ligament-related injury that you’ve probably heard of is called adhesive capsulitis. More commonly known as frozen shoulder, adhesive capsulitis is a condition involving pain and stiffness in the shoulder joint. It starts off gradually, but gets worse as time goes on.
Frozen shoulder develops when the connective tissue around your joint becomes thick, stiff, and inflamed. This includes the ligaments that connect your upper arm bone (humerus) to your shoulder socket (glenoid) and the capsule that holds them all together. Remember that ball and socket joint mentioned earlier in the article?
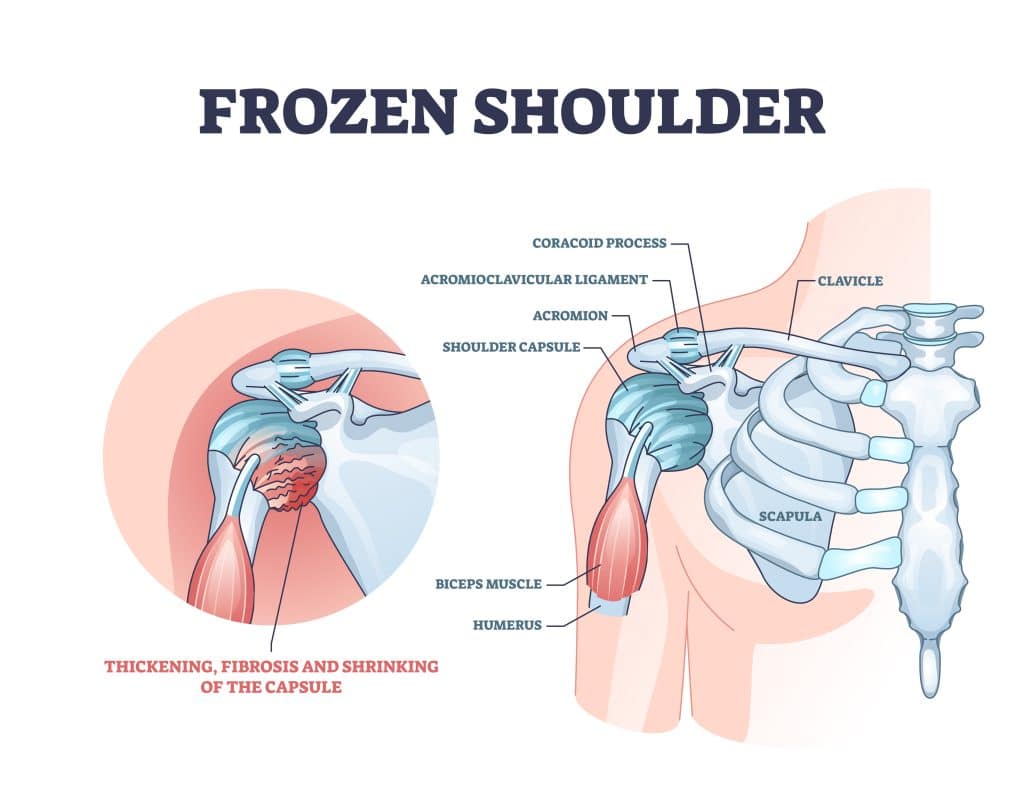
It’s called “frozen” shoulder because the more your shoulder hurts, the less you use it. And after you stop using it for a while, your shoulder capsule tightens, making it even harder to move- almost like it’s stuck or frozen in place.
Symptoms:
There are 3 stages to frozen shoulder.
- Stage 1: This is called the freezing stage, where your shoulder becomes stiff and it hurts to move. The pain will slowly get worse, especially later in the day. It will also start to be more difficult to move your shoulder. All in all, this stage lasts anywhere from 6 weeks to 9 months.
- Stage 2: This is known as the frozen stage, where your pain might not be as bad as before, but the stiffness still remains. Regular daily tasks and activities will start to become more challenging too. This stage lasts around 2 to 6 months.
- Stage 3: This is referred to as the thawing stage, where your pain and stiffness slowly begins to improve. A full recovery (or close to it) is when you regain your normal strength and range of motion. This stage can take 6 months to 2 years to complete.
Causes:
Experts aren’t exactly sure why frozen shoulder happens. It develops when swelling causes the joint capsule in your shoulder to tighten and thicken. Over time, scar tissue forms and there’s less synovial fluid to keep the joint lubricated. All of this makes it harder for your shoulder to move and rotate like it should.
There are a few risk factors that increase your likelihood of getting frozen shoulder. It usually affects adults, more often women than men, between 40 to 60 years old. Around 20% of diabetics also develop adhesive capsulitis at some point. Other health conditions, like heart disease and stroke, are risk factors as well because they may limit how much you move your arms and shoulders.
If you’ve had a recent shoulder injury, especially one that requires you to keep your shoulder still (like with a brace or sling), then your risk for developing adhesive capsulitis increases. Some examples of these types of injuries include collarbone fractures and even rotator cuff tears.
Diagnosing:
In order to diagnose frozen shoulder, your doctor will review your symptoms and medical history. They’ll check your passive range of motion by moving your shoulder in different directions to see how far it moves with and without pain. They’ll also watch you move your shoulder on your own without any assistance, which is your active range of motion, and compare the two. If you do have a frozen shoulder, then both types of movement will be quite limited.
Your doctor may order imaging to help rule out other reasons for your pain and stiffness. X-rays can spot things like arthritis and any issues with your bones, whereas an MRI can identify soft tissue injuries in your shoulder, like a torn rotator cuff.
Treatment:
One of the best ways to treat your frozen shoulder is with physical therapy. Treatment will initially focus on managing your pain while you’re still in the “freezing stage”. Your sessions will include different kinds of stretches and mobility exercises, like external rotation, forward flexion, and a crossover arm stretch.
Your physical therapist will also give you exercises that focuses on your range of motion. They’ll help you work through the “frozen stage” of your condition until your movement’s restored. The great thing about the exercises they give you is that you can do them safely at home so you can keep making progress even on the days you don’t have therapy.
You can lower your risk of frozen shoulder by starting physical therapy right after any injury that makes it difficult or painful to move your shoulder. The physical therapist can create a custom exercise plan that works best for you.
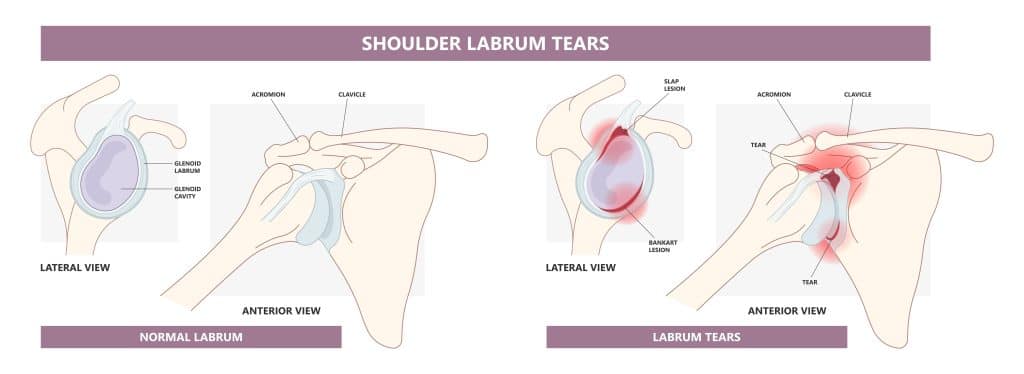
Labrum Tear
Your labrum is a thick piece of cartilage that sits along the edge of your shoulder socket. It has two main jobs: it deepens the socket so the ball of your shoulder stays in place, and it also acts as an important attachment site to the ligaments that help hold your joint together. If you tear those ligaments during an injury, your labrum can sometimes tear away from the bone too.
This usually happens when you dislocate your shoulder, especially if it’s a result of some kind of trauma. In these types of cases, the ball of your humerus can pop forward toward the front of your body (called anterior dislocation) or toward the back (called posterior dislocation.) In both instances, the labrum still gets torn off the bone and usually doesn’t heal back in the right spot.
Symptoms:
Like with any tear, the most common sign of a labrum tear is pain and instability. Sometimes there can be a grinding, locking, or catching sensation when you move your shoulder. Symptoms vary from person to person though, depending on the type of tear.
Baseball players are no strangers to labrum tears. Especially with all of the repetitive motions they have to do on a daily basis. Most of them feel pain while throwing, especially as they release the ball. They also usually notice some issues with their biceps as well, like trouble with their follow through.
Causes:
Two of the most common labral tears are SLAP tears and Bankart tears. Both of these tears are painful and make your normal everyday shoulder movements more difficult to do.
The term “SLAP” stands for Superior Labrum from Anterior to Posterior. SLAP tears are a type of tear that happens near the front (anterior) of your arm, where your shoulder and biceps tendon meet. Pitchers, lacrosse players and volleyball players are prone to SLAP tears because they have to do fast snapping movements. These high energy motions that go over the top of their shoulders take a toll over time, which can lead to tearing.
Typically, Bankart tears happen when you dislocate your shoulder. Essentially what happens is as the ball of your shoulder joint pops out of the socket, the tissue around your joint can pull on the labrum and actually tear it. Once this happens, your shoulder isn’t as stable as it should be, which means you could dislocate it again.
Types Of Labrum Tears
Labrum tears can take a few different forms.
The first type involves the labrum tearing completely off of your bone. This usually happens when you dislocate or subluxate your shoulder. In some cases, you won’t even realize you have a tear or that your shoulder has slid out of its socket.
The second type of tear is within the labrum itself. Over time, the smooth edge of your labrum can start to fray and then eventually tear. These tears are actually pretty common, especially for adults over 40, and typically don’t cause any symptoms.
The last type of tear happens in the area where your biceps tendon connects to the upper part of your shoulder socket. The biceps tendon blends in with your labrum, so if the biceps tendon gets injured, then the labrum can get injured too. The complexity of the tear can range anywhere from mild to severe.
Diagnosing:
It’s tough to diagnose a tear by examination alone, since your labrum is deep inside your shoulder. There are a few tests that your doctor can perform, but they’re not always reliable. Plus, some of the tests only identify one kind of tear but not the others.
Imaging, like MRI’s, are relatively good at showing whether there’s a labrum tear, but once again, they’re only around 85% accurate and that’s only if the tear was caused by a dislocation or subluxation. The best way to confirm a labrum tear is with a CAT scan where they inject dye into your shoulder.
Treatment:
When it comes to treating a labrum tear, it all depends on which type of tear you have. Some of them can heal on their own (with time). Frayed labrums usually aren’t bad enough and don’t need any type of invasive treatment. More severe tears, like if your labrum is completely torn from the bone, will need surgery to get reattached. A moderate sized tear may just need to get trimmed and cut out.
Whether you need surgery or you don’t, the most important part of your recovery will be to work on stabilizing your shoulder. With physical therapy, you’ll learn how to move your shoulder in a safe yet effective way.
Your therapist will create a customized exercise program specifically for you and your injury. These exercises focus on strengthening the muscles surrounding your shoulder joint that help keep it in place. The PT will also modify the way you do some of your daily activities or tasks so they’re less risky to your shoulder. As you heal, you’ll have less and less restrictions, until you’re to the point where you can safely return to doing all the things you love doing.
Generally, it takes about 4 to 6 weeks for your labrum to reattach itself to the bone, and then another 4 to 6 weeks to start seeing some strength come back. After that initial 6 weeks, you’re good to go with starting therapy and getting on the road to recovery.
AC Joint Sprain
The AC joint, or acromioclavicular joint, is where your collarbone and shoulder blade meet. 3 ligaments connect the two bones together near the top of your shoulder. If these ligaments get damaged, then you have something called an AC joint sprain.
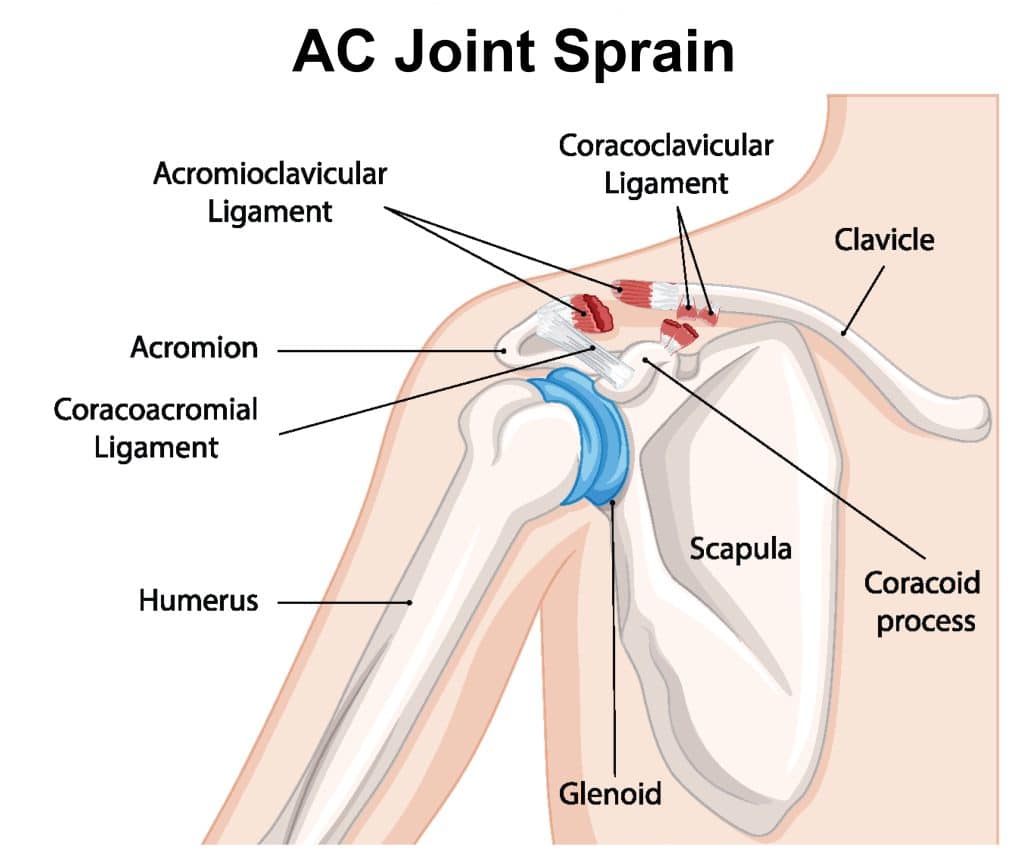
Your AC joint keeps your shoulder in its proper spot. But, it’s the capsule and ligaments job to create stability inside your AC joint so it can work properly. If either of them get injured, then your joint becomes unstable, which can be painful. It’s actually pretty easy for your ligaments to stretch and even tear if it goes through enough trauma. Like if you accidentally fall, the impact against the ground can cause your shoulder (and ligaments) to stretch beyond what they’re used to and they could end up tearing.
Symptoms:
Usually with an AC joint sprain, you’ll have pain near the top of your shoulder and sometimes there will be swelling and tightness too. It varies depending on how serious your injury is. With a mild sprain, you may only notice a little bit of pain and swelling, whereas a full ligament tear can cause intense pain and leave you unable to move your shoulder. Certain movements can also make your pain worse, like crossing your arms in front of your body or lifting them overhead.
Grades Of AC Joint Sprains
AC joint sprains are graded based on how severe the ligaments are stretched and torn.
Grade 1. Grade 1 sprains are the mildest of the 3 grades. It’s a gentle sprain where your ligaments are stretched out but not torn yet. Typically, there’s only a bit of pain and swelling, and you’re still able to use your shoulder.
Grade 2. A grade 2 sprain is when there’s a partial tear in your ligament and possibly a slight separation of your AC joint. With these kinds of sprains, it can be difficult to use your shoulder, and you might get pain even when you’re not moving it.
Grade 3. Grade 3 sprains happen when you completely tear or rupture one of your ligaments. You’ll likely notice a bump on your shoulder from your shoulder blade and arm bone moving. There’s usually some pretty severe pain and swelling with grade 3’s. And since the strength of your ligament is now hampered, it can be really difficult to move your shoulder even a small amount.
Causes:
One of the most common causes of AC joint sprains is from wear and tear, either by overuse or degeneration.
With overuse injuries, doing the same movements over and over at work or with normal daily tasks can strain your shoulder joint. After a while, your cartilage will wear down and your ligaments stretch out. Once you get to this point, that’s when you’ll start noticing signs of inflammation. It’s also pretty common for the AC joint to develop arthritis, which can cause degeneration in your joint.
You can sprain your AC joint from something as simple as an accident. Maybe you landed on your arm while trying to brace yourself from a fall or you took a hard hit to your shoulder after you misstepped and ran into a wall. It’s that type of sudden impact that pushes your shoulder blade away from your collarbone, which stretches and sometimes tears the ligaments that support your AC joint.
Diagnosing:
A physical exam is usually all that you need to diagnose an AC joint sprain. There’s a test that your doctor can do called the AC joint compression test. During the test, they’ll gently compress your AC joint with one hand on the front of the joint and the other on the back. If the movement causes pain, then that means you do in fact have a sprain.
Depending on your injury, you might need imaging to rule out any other issues with your shoulder. If your doctor’s worried that you may have a broken bone, they’ll send you to get some x-rays. If they’re concerned about the soft tissue around your joint, then an MRI is the way to go.
Treatment:
During the first 24 hours after you sprain your AC joint, you should rest and apply ice to help with any pain and limit your swelling. After that, you’ll want to begin physical therapy so you can keep your shoulder mobile while it heals.
In the beginning, you’ll do stretches and exercises that work on your range of motion. Your PT will help you modify your daily activities so you aren’t straining your ligaments or making your injury worse. As you progress, they’ll add in exercises that target the muscles that support your shoulder joint.
You should start to see improvement within the first week of therapy. Most people can make a full recovery, or at least close to it, within 6 to 8 weeks. If you have any other injuries to your shoulder, then it could take a couple of months before you’re able to return back to your normal activities.
Cartilage & Bone Injuries
Your shoulder joint features 3 bones: the arm bone, collarbone, and shoulder blade. At the ends of each bone is cartilage, which is a smooth layer of tissue that acts as a cushion. Thanks to cartilage, your bones can move freely and with very minimal friction.
Shoulder Dislocations
Shoulder dislocations happen when you pop the bones in your shoulder joint out of place. There are different shoulder joints, the acromioclavicular joint and the glenohumeral joint.
The joint that dislocates most often is your glenohumeral joint. It’s made up of two bones: the upper arm bone, or humerus, and the shoulder blade, or scapula. The end of your humerus is shaped like a ball and fits into the part of the scapula that resembles a socket. It’s when the connection between these two bones is separated that a dislocation happens.
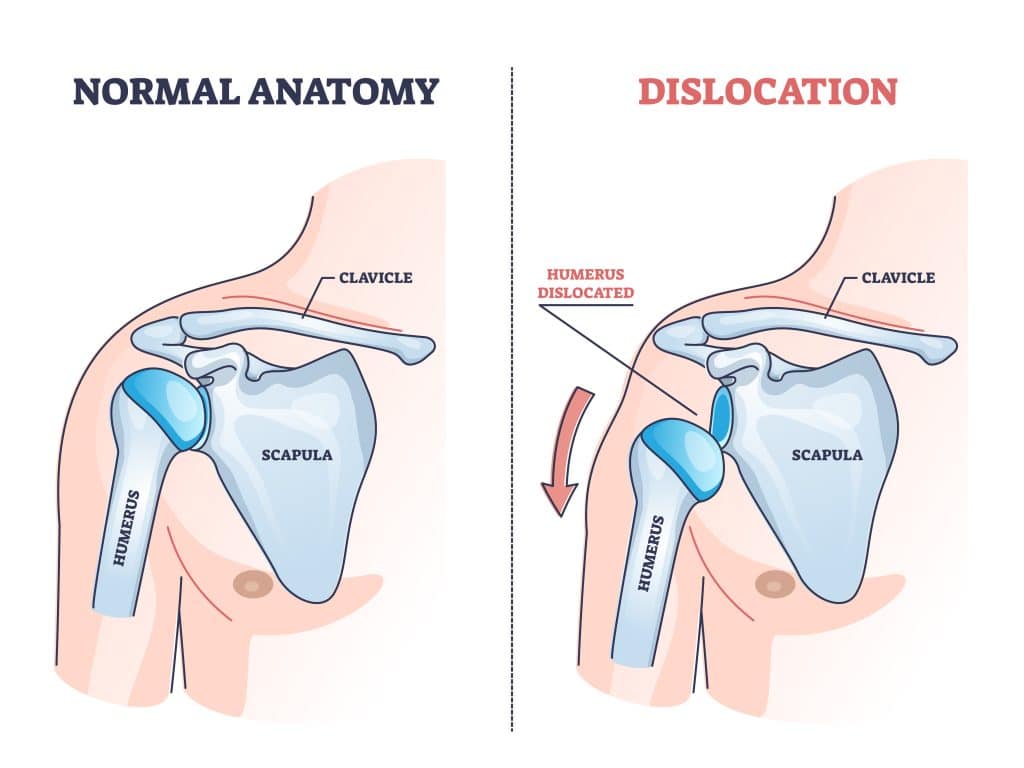
There are 2 types of dislocations, which are based on how far the bones in your joints have moved. The first type is a partial dislocation, also called a subluxation. Your shoulder is subluxated if your joint is pulled apart, but the bones are still touching. The other type of dislocation is a complete dislocation, or luxation. If your bones are totally separated and pushed out of place, then your shoulder is luxated.
Symptoms:
Shoulders are the most frequently dislocated joint in the body, which is no surprise since they can move in so many different directions. Dislocations can happen forward, backward, and even downward. Consequently enough, the nearby muscles, tendons, and ligaments can easily get damaged in the process.
When you dislocate your shoulder, the first thing you’ll notice is it visibly out of place. You also won’t be able to move your arm. Shortly after that, the pain, swelling, and bruising kicks in. Don’t be surprised if you feel some numbness or tingling around your neck and down your arm either. Sometimes your shoulder muscles can spasm, which can make your pain even worse.
Causes:
Most shoulder dislocations happen in the forward direction towards the front of your body. At the same time, the ligaments around your shoulder can stretch and tear, which would make your dislocation even worse.
There needs to be some sort of strong force, like a sudden hit to your shoulder, for your bones to get pushed out of place. Your arm bone can also pop out of its socket if there’s an extreme amount of twisting on your shoulder joint too.
That being said, it’s ultimately traumatic, direct impacts that cause the most dislocations. This can be something like being in a collision while driving or taking a hard blow during contact sports. Falls are another big one, either by landing awkwardly or sticking your arm out in an attempt to brace yourself. It doesn’t even have to be a big fall either. You can trip on a loose rug or fall off of a step stool and still end up dislocating your shoulder.
Everyone is capable of dislocating their shoulder, but some people are more at risk than others. Men are twice as likely compared to women. Younger adults between ages 15 to 30 and anyone with a history of shoulder dislocations also have a higher potential as well.
In most cases, when you dislocate your shoulder, the area surrounding your joint suffers the same fate. The damage can range anywhere from a ligament sprain to a fractured bone or muscle strain. Not to mention, if your humerus is in the wrong position, you could end up developing something called a Hill-Sachs lesion. More on that later, though.
Diagnosing:
Unlike some injuries, diagnosing a shoulder dislocation is usually pretty straightforward. Your doctor will look for the tell-tale visible deformity of your arm sitting out of its socket. Another obvious is if you’re unable to move your arm, since everything is out of place. If your doctor is worried about other areas of your shoulder being damaged, then they might order an MRI or x-ray.
Treatment:
As for treating shoulder dislocations, the most important thing you need to do before anything else is get your arm back into the socket. Don’t try to be a hero and do this yourself though. It might look easy on tv and in the movies, but you can easily make your injury way worse (not to mention, more painful!)
In order to get your shoulder back in place, your doctor will perform something called a closed reduction. Basically, they’ll push on one area of your body (usually around your armpit area) while pulling on your arm until the shoulder is set. Once that’s taken care of, you’ll have to wear a sling to keep your shoulder immobilized so it can heal. You’ll also need to start physical therapy fairly soon after that. The longer you wait, the more your shoulder will freeze and tighten up.
The first thing your physical therapist will do is go over all the activities you need to avoid (at least temporarily) so they don’t strain your shoulder. In the beginning, you’ll only be doing gentle movements that help with the stiffness.
As your ligaments heal, you’ll get new exercises that focus on strengthening the muscles that support your shoulder joint. Keeping up with these exercises will help prevent more dislocations from happening in the future. All in all, most people are able to return to their normal activities after 3 to 4 months of therapy.
Hill-Sachs Lesion
A Hill-Sachs lesion looks similar to a dent, but it’s actually a compression fracture on the back of your upper arm bone that develops after you dislocate your shoulder. Basically, when your shoulder is dislocated, the humerus can slip and press against the edge of the joint socket, which can damage the top of that ball-shaped bone.
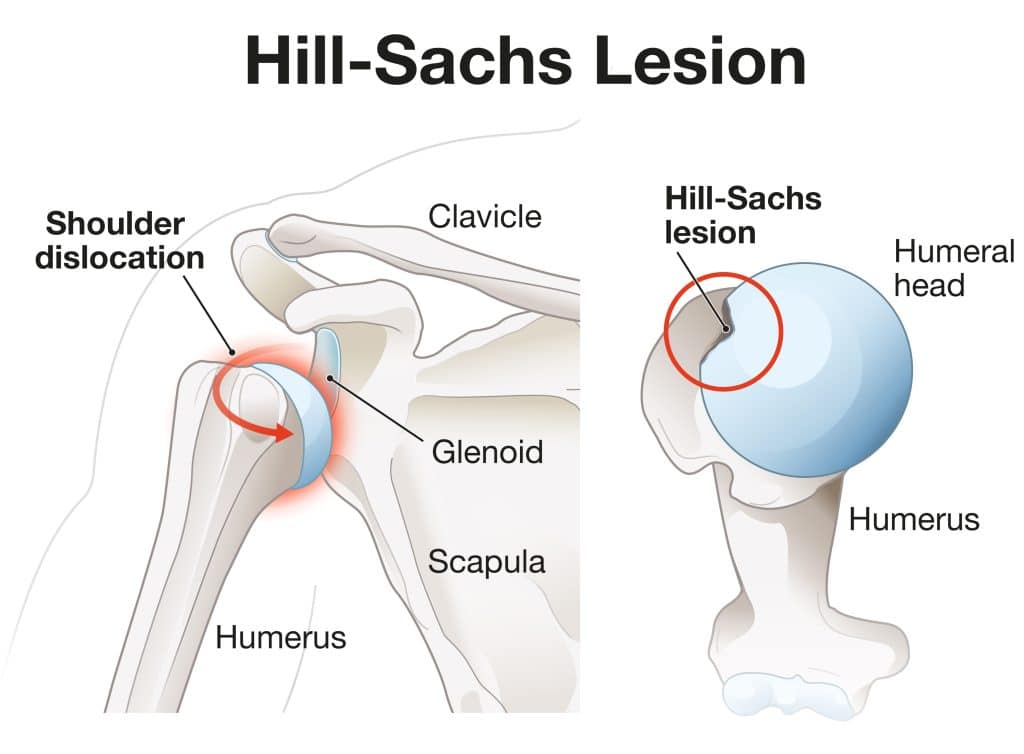
Anyone with a dislocated shoulder can develop a Hill-Sachs lesion. Some people have a higher risk for dislocations than others, which means those people are also more likely to develop a Hill-Sachs lesion afterwards too. Men, athletes in contact sports, and anyone with a history of dislocations are more at risk.
When you get a Hill-Sachs lesion, it’s nearly impossible to move your arm, especially right after the dent appears. In the rare event you are able to move it, it’s usually extremely painful and very uncomfortable. A lesion can also make your recovery take longer than it normally would with a typical dislocation.
Symptoms:
Most of the time, Hill-Sachs lesions have the same symptoms as the dislocation itself. This includes a lot of pain, swelling, bruising, weakness, and sometimes numbness or tingling down your arm and into your hand.
Hill-Sachs lesions are graded by how deep the lesion is. Generally, the higher the grade of the lesion, the higher your risk of experiencing another dislocation. With a grade 1, there’s a defect in the articular surface. When the lesion includes the subchondral bone, it’s a grade 2. And a grade 3 Hill-Sachs lesion means there’s a large defect in the subchondral bone.
Another way to classify Hill-Sachs lesions is whether they are “on” or “off” track. If the lesion goes beyond your glenoid track, then it’s considered engaging or “off track”. If it stays within your glenoid track, then the lesion is non-engaging or “on track”.
Causes:
The only way to get a Hill-Sachs lesion is by dislocating your shoulder. If the dislocation is forward, meaning it’s away from the front of your body, then the rounded ball part of your humerus can press against the lip of the socket joint. Over time, the pressure can create a dent in your bone.
Diagnosing:
Your doctor can diagnose a Hill-Sachs lesion by taking a look at your dislocated shoulder. They’ll also use imaging, like x-rays or MRI’s, to get a better idea of the kind of damage you have inside your shoulder joint.
Treatment:
The size of your lesion will determine what kind of treatment you’ll need. If it’s less than 20% of your humeral head, then you’ll treat your injury just like a simple shoulder dislocation.
The most important thing is to take care of the dislocation and get your shoulder bone back in its socket. This is where the doctor does something called a closed reduction. Think of all those scenes on tv where the doctor pushes and pulls your arm until it snaps into place.
After your shoulder is aligned again, you’ll likely have to keep it in a sling so everything can heal properly. In the same regard, you don’t want to be completely immobile to the point where your shoulder freezes or tightens up either. It’s a tricky balance, but physical therapy can help you navigate your way through.
In the beginning, you’ll focus on gentle stretches that keeps your shoulder flexible and prevents it from stiffening up. You’ll also have to change up how you do some of your typical daily activities, like getting dressed or chores around the house. Your PT will work with you to figure out the best way to do these movements, but in a safe way.
Over time, you’ll get more strengthening exercises to build up your muscles and test your ligaments. All of this will help stabilize your shoulder and reduce your risk of dislocating it again in the future. It takes most people several months of physical therapy to fully recover from a Hill-Sachs lesion and shoulder dislocation.
Shoulder Fractures
As you probably remember, there are 3 bones that make up your shoulder joint: the arm bone, collarbone, and shoulder blade. When one of them breaks, then you have something called a shoulder fracture (which is the medical term for a broken bone).
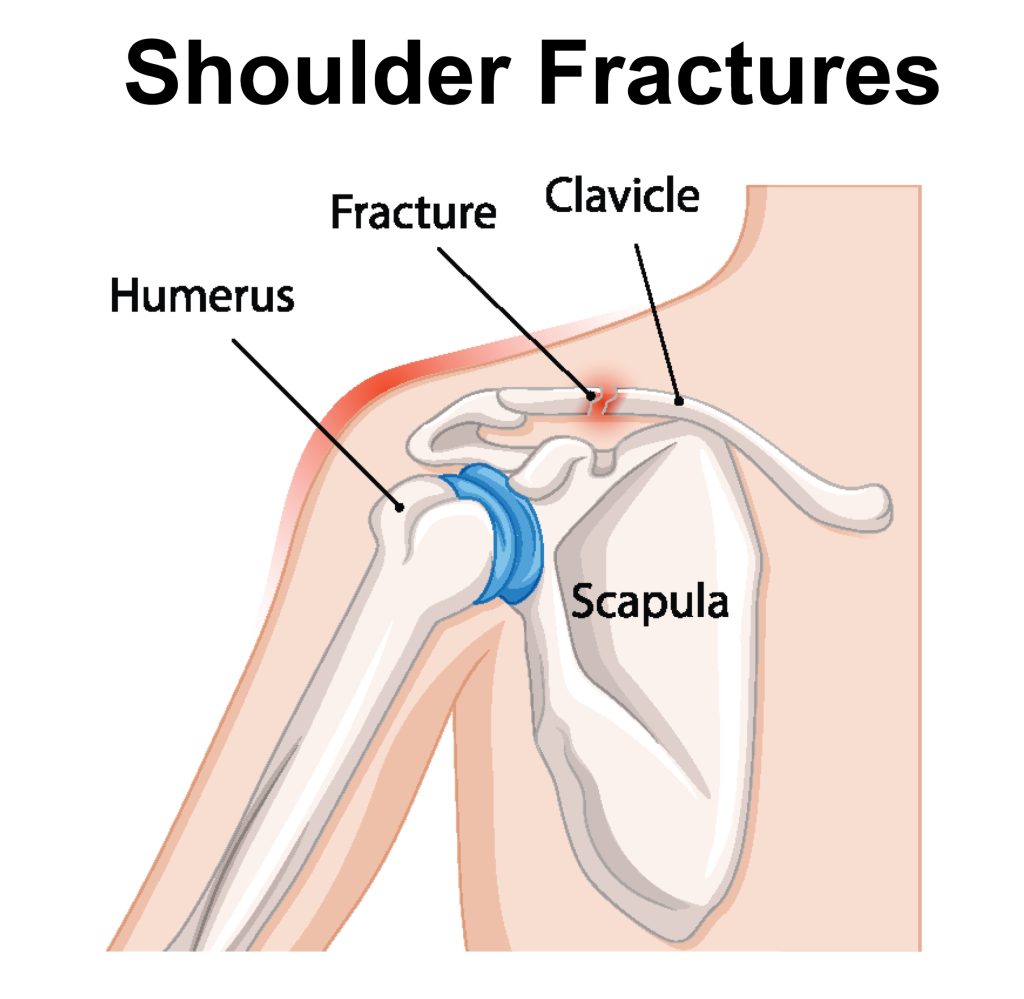
Shoulder fractures aren’t very common, especially compared to other injuries like dislocations or shoulder separations. Of the 3 bones, adults are more likely to fracture their arm bone. Teens, on the other hand, usually break their collarbones. It’s pretty hard to break your shoulder blade since it’s protected by muscles on both sides.
There are 4 different kinds of shoulder fractures: displaced, non-displaced, open, and closed.
If you have a displaced fracture, the pieces of your broken bones have shifted so much that there’s large gaps in between them now. With non-displaced fractures, the pieces haven’t moved too far, so the bones are still in alignment. Then there’s open fractures, which means your broken bone sticks out through your skin. Closed fractures are still serious but the broken bone stays under your skin.
Symptoms:
Anyone who’s ever broken a bone before knows it can be pretty painful, and your shoulder is no different. You also won’t be able to move or use your arm very well because of it. There’s typically swelling and some bruising or discoloration that shows up shortly afterwards too.
A lot of people with shoulder fractures end up dealing with at least a little bit of permanent stiffness, even after their break has healed. Unfortunately, your fracture also increases your risk of eventually developing arthritis in that shoulder.
Causes:
Almost all shoulder fractures are caused by some kind of sharp abrupt impact that has a lot of force behind it. This can be anything from a fall to a car accident.
It’s mostly elderly adults with a history of falling that fracture their shoulders, but it can happen to anyone. It’s even worse if you have osteoporosis or osteopenia because your bones are naturally weaker and easier to break.
Diagnosing:
Your doctor can tell if you have a fracture by carefully examining your shoulder. They’ll order x-rays to see how much damage there is to your bones and possibly even an MRI to check the cartilage and ligaments around it.
Treatment:
The type of treatment you’ll need all depends on which bone is broken and if there’s any other damage to worry about. If it’s a mild fracture and the broken pieces haven’t moved much, then you’ll likely just need a sling so everything stays in place and heals properly. You’ll have to be cautious with this though. Keeping your shoulder still for extended periods of time can end up creating more issues down the line. You want to prevent your broken bones from shifting, but at the same time, keep the muscles that support your shoulder joint strong. That’s where physical therapy comes in.
During PT, your physical therapist will help you regain mobility in your shoulder while still being mindful of your fracture. They’ll create a specialized exercise program that focuses on getting your strength and range of motion back up too. It might not seem like a whole lot in the beginning, but they’ll add on more exercises as you progress.
If your fracture is severe enough, you run the risk of permanent stiffness in your shoulder. That’s why it’s important to start physical therapy sooner rather than later.
Joint Arthritis
Another shoulder injury you might experience is joint arthritis, which can happen to both the AC joint and glenohumeral joint. As the name suggests, joint arthritis is a condition where you develop arthritis in at least one of your joints. It usually affects adults over 50 and anyone with a history of traumatic shoulder injuries.
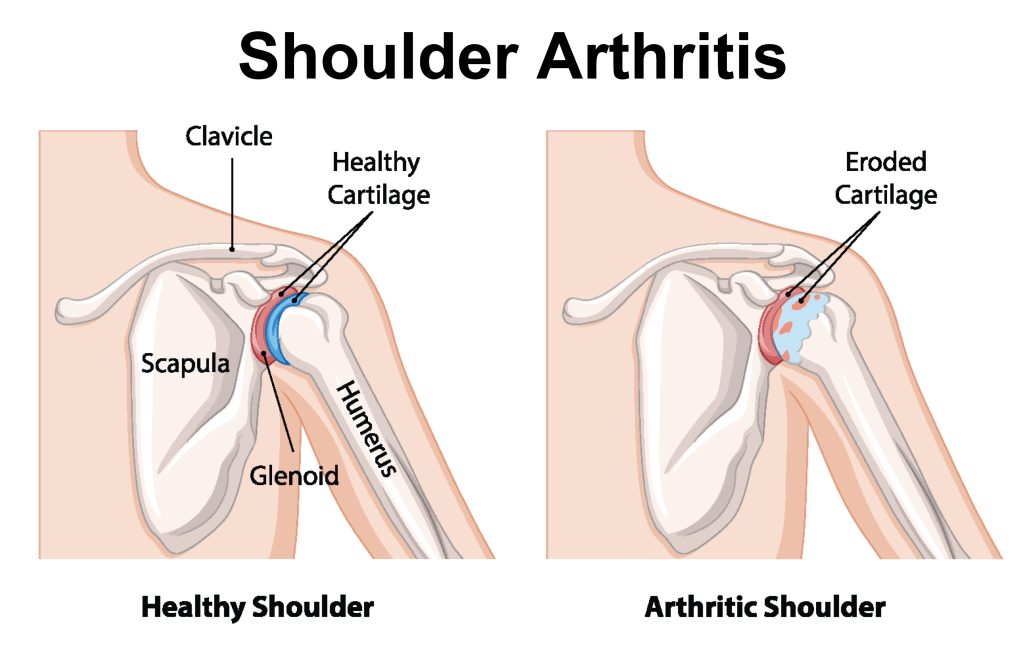
When there’s arthritis in your shoulder joint, it’s the inflammation that causes the pain and makes it uncomfortable to move your arm. Likely, you’ll notice pain when you’re lifting something heavy or reach overhead. Severe cases can make even the simplest everyday tasks, like using a computer or getting dressed, impossible to do.
Over time, arthritis wears down the cartilage lining your joint. If you remember from earlier, cartilage is that cushiony layer covering your bones that lets you move your shoulder so smoothly. Once that protective cartilage is gone, that’s when your bones start rubbing against each other.
Arthritis develops in 4 stages. In the first stage, your cartilage gets soft. Next, it will start to develop cracks. Then, it will deteriorate and flake off. Finally, the cartilage wears down to the point where the surface of your bone is exposed. It’s at this stage that your joint is no longer able to glide effortlessly.
There’s nothing uniform about the way cartilage gets worn down. Instead of the entire surface wearing away all at once, different parts wear down at different rates, similar to how swiss cheese looks.
There’s no way to tell how quickly it will take for your arthritis to get worse. Generally, when activities start causing you pain, it’s an indication that there’s stress on your cartilage. And in most cases, the more painful the activity is, the more damage there is to your cartilage and shoulder joint.
Symptoms:
One of the most universal signs of arthritis is joint pain. When you have arthritis in your shoulder, you’ll feel it in the front, back, or side. At first, it might only be painful when you’re being active, but as the arthritis progresses, you’ll start to feel it at any point throughout your day, even when you’re not moving your arm. You’ll notice the pain gets worse after you exercise or do any heavy lifting. It may even start to spread down your arm into your wrist if the arthritis is bad enough.
With arthritis typically comes stiffness as well. The two tend to go hand in hand. You might not be able to move your shoulder like you used to because of that stiffness, which can make things like driving or getting dressed pretty challenging. Stiffness is also a big indication that your arthritis is getting worse.
It’s also not uncommon to experience clicking, grinding, or popping noises in your shoulder. That’s because the arthritis has worn down the cartilage so much that it’s not smooth anymore. Now instead of gliding easily, the joint makes all these noises. Your shoulder might also slide when you move certain ways or even lock up sometimes too.
Causes:
Osteoarthritis is the most common type of arthritis. This is that wear and tear type of joint disease you get as you age. Basically, your cartilage gets soft and starts to crack, flake or fray. Eventually the cartilage wears away, leaving the bone underneath exposed to rub and grind against one another.
Rheumatoid arthritis, or RA, is a different type of arthritis you can get in your shoulder. RA is an autoimmune disease, which is just a fancy way of saying that your body’s natural defense system attacks its own healthy tissues. With your shoulder, your joint and its lining are being attacked, which causes the lining to swell. Eventually, your cartilage will get damaged in the process.
Another thing that can lead to shoulder arthritis is a rotator cuff tear. Your rotator cuff stabilizes your shoulder and keeps that ball and socket joint in place when you move. Over time, those tendons can wear down and begin to tear. If the tears get big enough, the humeral head can start to slide out from its normal position and rub against your shoulder blade, which causes arthritis.
Diagnosing:
In order to tell whether there’s arthritis in your shoulder, a doctor will test your strength and range of motion. They’ll also order imaging as well.
Even though x-rays only show bone and not cartilage, your doctor will still be able to see how much space is between your bones. If they’re touching, or very close to it, then that means your cartilage has been worn down, likely from arthritis. They might send you to get an MRI too if they’re worried about the condition of your rotator cuff tendons.
Treatment:
The key thing to know about arthritis is that it’s very important to keep your shoulder moving so it doesn’t lock up, even though it might not feel the greatest in the beginning. With the help of physical therapy, you can learn to manage your symptoms while still maintaining mobility.
Your therapist will teach you different stretching exercises that work on improving your range of motion. The great thing about these exercises is that you can always do them again in the future if your shoulder starts to bother you.
If you haven’t lost any range of motion yet, then your goal is to prevent your shoulder from deteriorating. It’s usually a gradual thing when you lose the motion in your shoulder joint, so it can be a bit hard to notice if you’re not looking for it. It’s only when you’re not able to be as active and your pain has increased that you realize your joint is getting stiffer.
Depending on your job and hobbies, you may have to make some changes or adjustments so you don’t hurt your shoulder. Your physical therapist will help you modify these kinds of activities, like lifting heavy objects or certain household chores, so you’re able to do them without causing pain. They’ll also add some strengthening exercises to your program so the muscles that support your shoulder joint are stable and strong.
If your arthritis becomes severe enough, your doctor may suggest steroid shots or even surgery. While there’s no cure for arthritis, you can learn to treat your symptoms and still have an active, enjoyable life.
Shoulder Bursitis
As the name suggests, shoulder bursitis is bursitis in your shoulder joint. The technical term for this is subacromial bursitis. Basically, it’s inflammation in the bursa, a fluid filled sac between your shoulder blade and rotator cuff tendons. It’s caused by irritation or damage to the bursa, which in turn leads to pain and swelling.
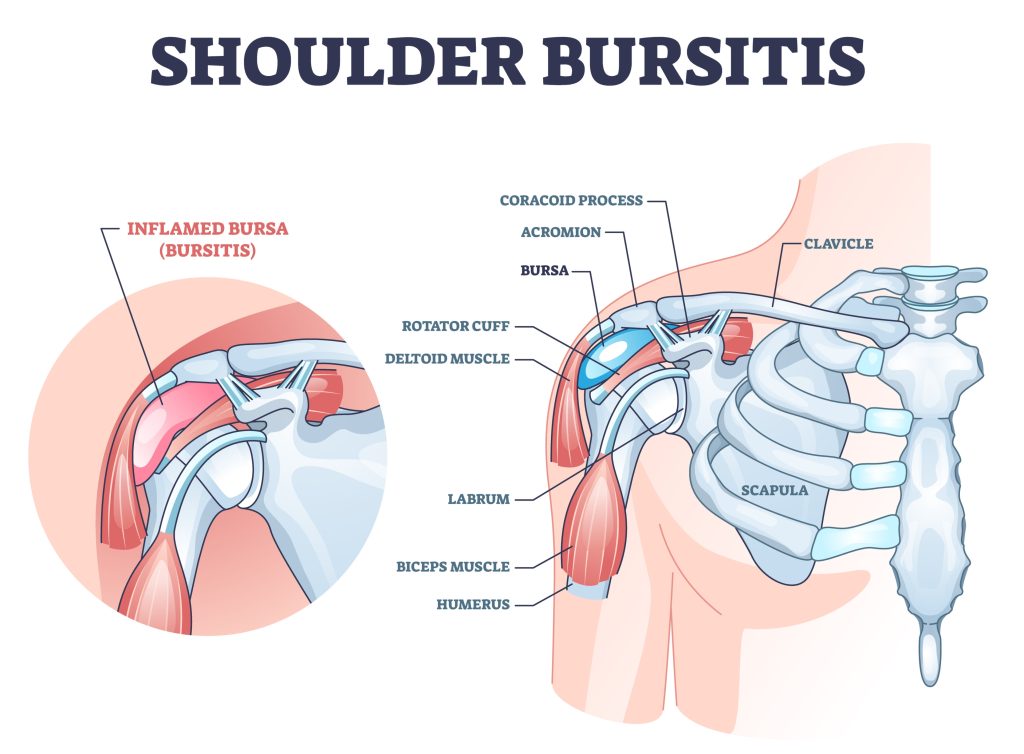
There are 3 types of bursitis: chronic, acute and septic.
Chronic bursitis is when you keep getting episodes of bursitis in your shoulder, usually from overuse. It’s the most common of the 3 types. Acute bursitis is a stand alone incident that happens suddenly, typically after you get injured. Septic bursitis happens when there’s an infection somewhere in your body and it eventually makes its way to the shoulder bursa.
Symptoms:
Most people with shoulder bursitis experience pain, stiffness, and swelling. You can have a limited range of motion as well. The pain may come on all of a sudden or build up over time, and is typically worse at night. You might also feel a dull ache throughout your day or get a sharp pinchy feeling when you move your shoulder certain ways.
Causes:
Shoulder bursitis is usually caused by overuse or from an injury. Essentially, anything that damages your shoulder can create inflammation and irritate your bursa.
Doing the same movements over and over again, either at work or during sports, can start to wear on your shoulder. At first, you may not notice any pain, but if you do the those motions often enough, you might not be giving your shoulder enough time to fully recover. Eventually, the irritation builds up and ends up causing bursitis.
Anyone can get bursitis, but some things can put you at a higher risk. Playing sports that have repetitive movements, like swinging a club or throwing a ball, is a big one. Physically demanding jobs is another. Working with tools or lifting heavy objects every day puts a lot of stress on your shoulder. Arthritis, diabetes, and other health conditions may increase your likelihood of developing bursitis as well.
Diagnosing:
A doctor can diagnose shoulder bursitis by doing a few different tests, including checking your range of motion. They’ll also rule out any other injuries that could have similar symptoms.
You might have to get some imaging done too, like an x-ray to see if there’s bone spurs, or an MRI to look for inflammation. If those come back negative, your doctor will likely do a blood test to check for signs of some kind of infection in your body.
Treatment:
When you have bursitis, you’ll want to stop doing things that strain your shoulder. Your main goal is to give yourself time to heal while still remaining fairly active. With the help of physical therapy, you can work to strengthen your shoulder and improve your flexibility. More importantly, you’ll learn to manage your symptoms and how you can prevent future injuries as well.
Generally, it’s pretty rare to get surgery for bursitis. It’s more likely though if all other treatment options have failed and your bursitis is making it nearly impossible to do daily tasks. In this case, your surgeon would use a scope to go in and repair or remove the damaged tissue. They may even remove a portion of the bursa that’s swollen to create room inside your shoulder.
Click here to learn more about how Borja Physical Therapy can help treat your shoulder injury.