Did you know that your feet are one of the most vital parts of your body? Think about it. They support your body weight, allow you to stand, balance, and walk. They can even give you clues that you may have other health issues going on. Each foot is made up of muscles, tendons, ligaments, and bones, all packed into one little area. This article is going to explore the most common foot injuries and what you can do if you experience one yourself.
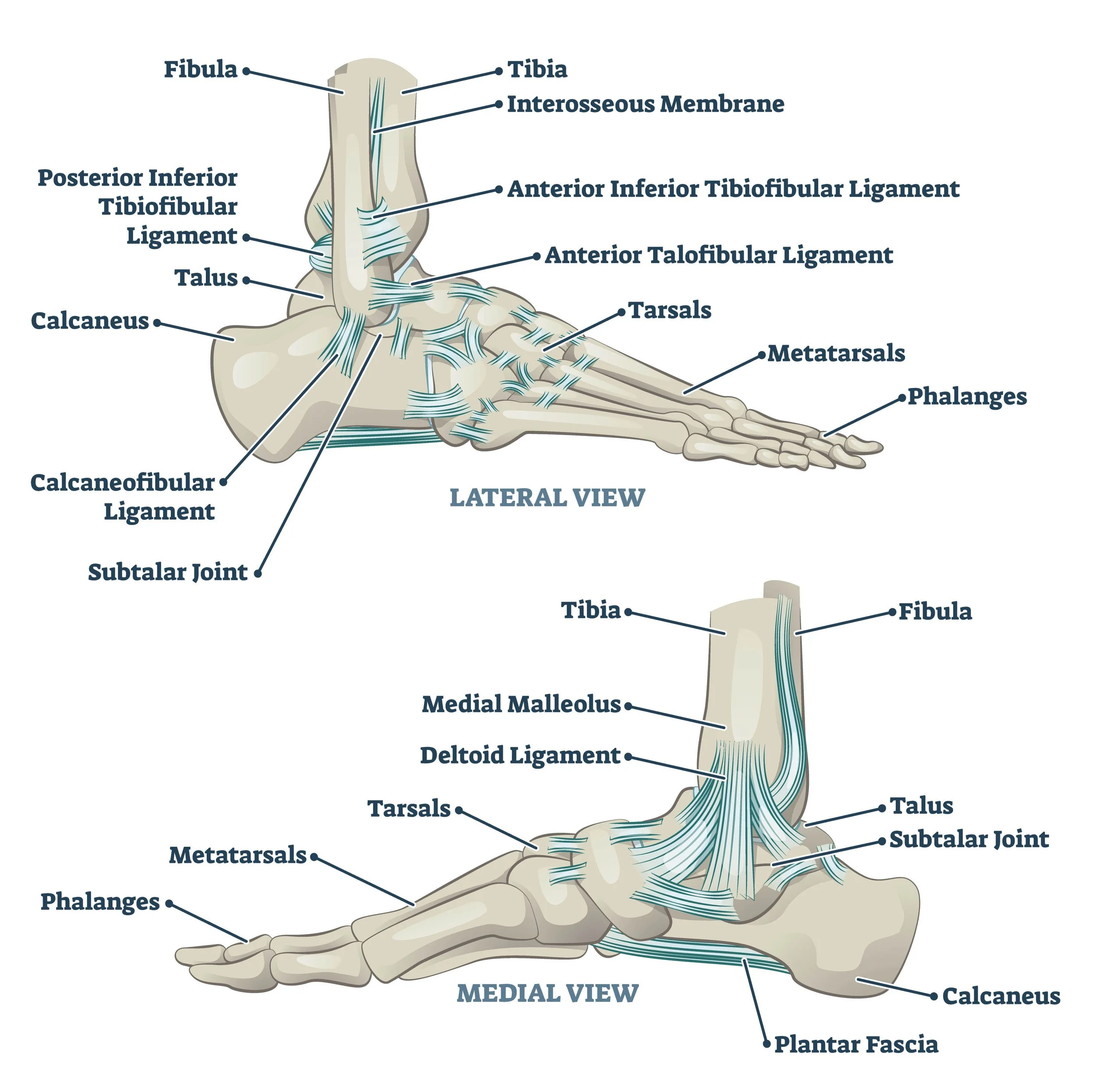
Let’s start at the beginning, with some basic anatomy.
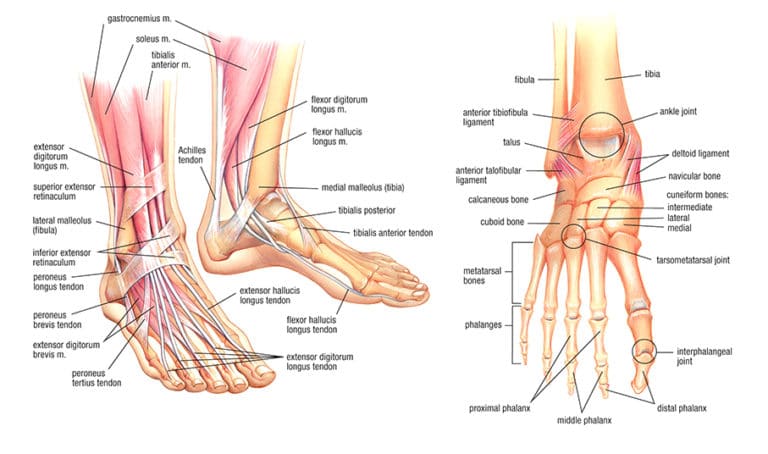
So, the picture might not look all that basic, but it shows you just how much you’ve got going on in such a small area like your foot. Of the 52 bones in the human body, your foot accounts for 26 of them. This includes the tarsals, metatarsals, and phalanges (which are the bones in your toes.) They’re all aligned in a way that creates 3 different sections: the hindfoot, midfoot, and forefoot.
Your foot is controlled by 13 extrinsic and 21 intrinsic muscles. Extrinsic muscles start in your lower leg and extend into your foot, whereas intrinsic muscles are solely located within the foot (pun intended.) Both groups of muscles work with their respective long tendons to maintain your arches and keep your foot stable.
All of your bones are connected together by 112 strong, flexible ligaments. There’s also a layer of cartilage covering the ends that acts as a cushion.
Now that you’ve got a better understanding of the different parts of your foot, let’s explore some common muscle and tendon injuries.
Muscles & Tendons
As you just read, there are a total of 34 muscles in your foot. They’re divided based on where the muscles start. The ones that come from your lower leg, called extrinsic muscles, are the reason you can do actions like inversion, eversion, plantarflexion and dorsiflexion with your foot. The muscles located completely within your foot, called intrinsic muscles, control fine motor actions, like wiggling your toes.
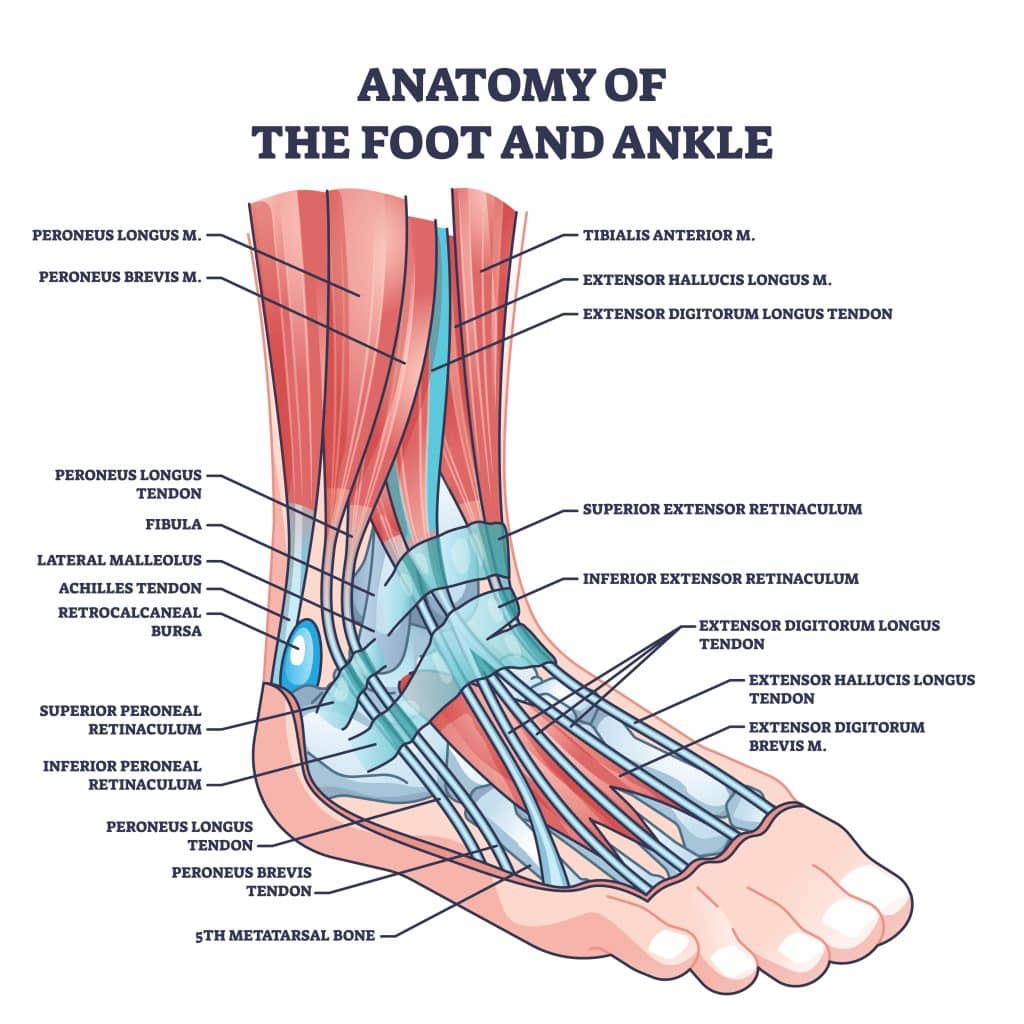
There’s also a number of major tendons in your foot, all of which play a huge role in how your foot moves. Some of the big name tendons include your Achilles tendon and your plantar fascia. You’ll learn more about these (and others) throughout this article.
Achilles Tendinitis
Let’s start with an injury almost everyone has heard of: Achilles tendinitis. Achilles tendinitis is inflammation of your Achilles tendon, which connects your calf muscle to your heel. You may hear it being referred to as “Achilles tendinopathy” which is just a more broad term used to describe this type of injury.
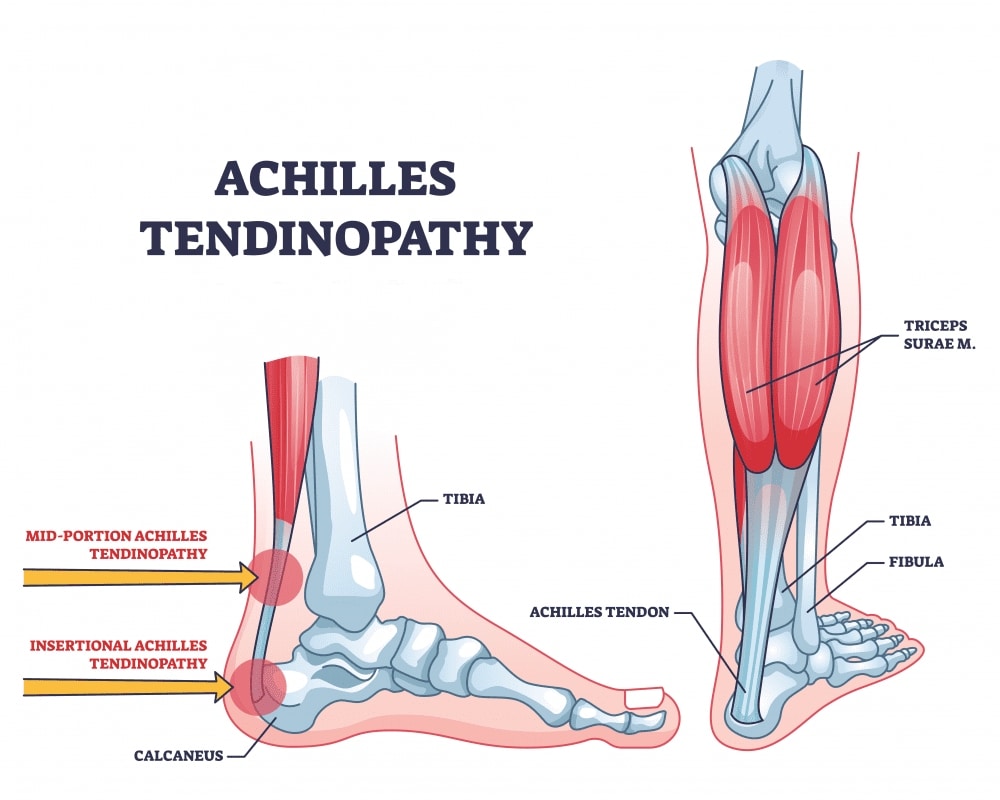
There are 2 types of Achilles tendinitis, noninsertional and insertional. It all depends on which part of your tendon is affected. With noninsertional, the middle of your tendon starts to break down, thicken and swell. Insertional Achilles tendinitis affects the part of your tendon that attaches, or inserts, near your heel.
Anyone can develop Achilles tendinitis, but it’s more common if you’re active. Nearly 25% of all athletes will get it at some point in their lifetime.
Symptoms
Since your Achilles tendon starts at the bottom of your calf muscle and runs all the way to your heel, that’s where you’ll find a lot of your symptoms.
Like with most injuries, the first that usually appears is pain, especially near your heel and ankle. Along those same lines is stiffness and swelling around your tendon. Don’t be surprised if your leg starts to feel a bit weak too.
You might notice some triggers that can make your symptoms worse. You’ll probably feel discomfort after you’ve exercised or if you’ve been more active than usual. Climbing up a bunch of stairs or going uphill can also cause things to flare up. For some people, the morning can be a bit rougher, but things usually improve as the day goes on.
Causes
Achilles tendinitis is generally an overuse issue. There doesn’t even necessarily need to be an accident type injury. Simply being active on your feet repeatedly stresses your tendon to the point that it starts to swell. And since it’s practically impossible not to use your Achilles, your body just doesn’t have enough time to repair the damaged tissue.
While Achilles tendinitis is common among athletes, it can really happen to anyone. Maybe you enjoying running through your neighborhood or have a job that requires you to be on your feet for long periods of time. You could even be what’s known as a “weekend warrior” where you’re only active one or two days a week, leaving your body less time to get used to all the stress. All of these things can lead to tendinitis.
For some people, they’re at a higher risk of getting Achilles tendinitis because of how their body is shaped and structured. For instance, having weak or tight calf muscles can keep your Achilles in a naturally stressed state. The same can be said about having flat arches or bone growths on your heel. Another big one is if you tend to overpronate, meaning your ankles roll inward as you walk.
Diagnosing
Diagnosing Achilles tendinitis can be done through a physical examination. Your doctor will ask about your symptoms and any recent activities where you’ve been on your feet a lot. They’ll look at your range of motion and check for signs of bone spurs or a ruptured tendon.
Treatment
It’s important not to ignore Achilles tendinitis or you could end up causing even bigger health problems for yourself. Luckily, it’s more than possible to recover from this kind of injury. Don’t wait too long though, because the longer you live with the pain, the longer (and harder) the recovery process will be.
The first thing your doctor will want you to do is the RICE method: rest, ice, compression and elevation. They’ll also recommend starting physical therapy. At PT, you’ll learn exercises and stretches that focus on regaining your strength, especially while you have to take it easy. They’ll teach you ones you can do at home too, so you’ll continue making progress on days you don’t have therapy.
One of the other things you’ll learn is what not to do. You want to protect your tendon as much as possible as it heals. This means avoiding overstretching your tendon (like while standing on the rung of a ladder) and walking up anything with a steep incline. You’ll also want some supportive shoes or orthotics. And absolutely no walking barefoot, even when you’re in your house.
It may take a couple months for your pain to start getting better, especially if you’ve been dealing with symptoms for a long time. Your therapist will help you throughout your journey, though.
Achilles Tendon Rupture
As you already know, your Achilles tendon goes from your calf muscle to heel bone. What you might not know is it’s the strongest and largest tendon in your body. It’s the whole reason your leg has the strength to walk, jump, and run. If you tear your Achilles tendon, then you have what’s known as an Achilles tendon rupture.
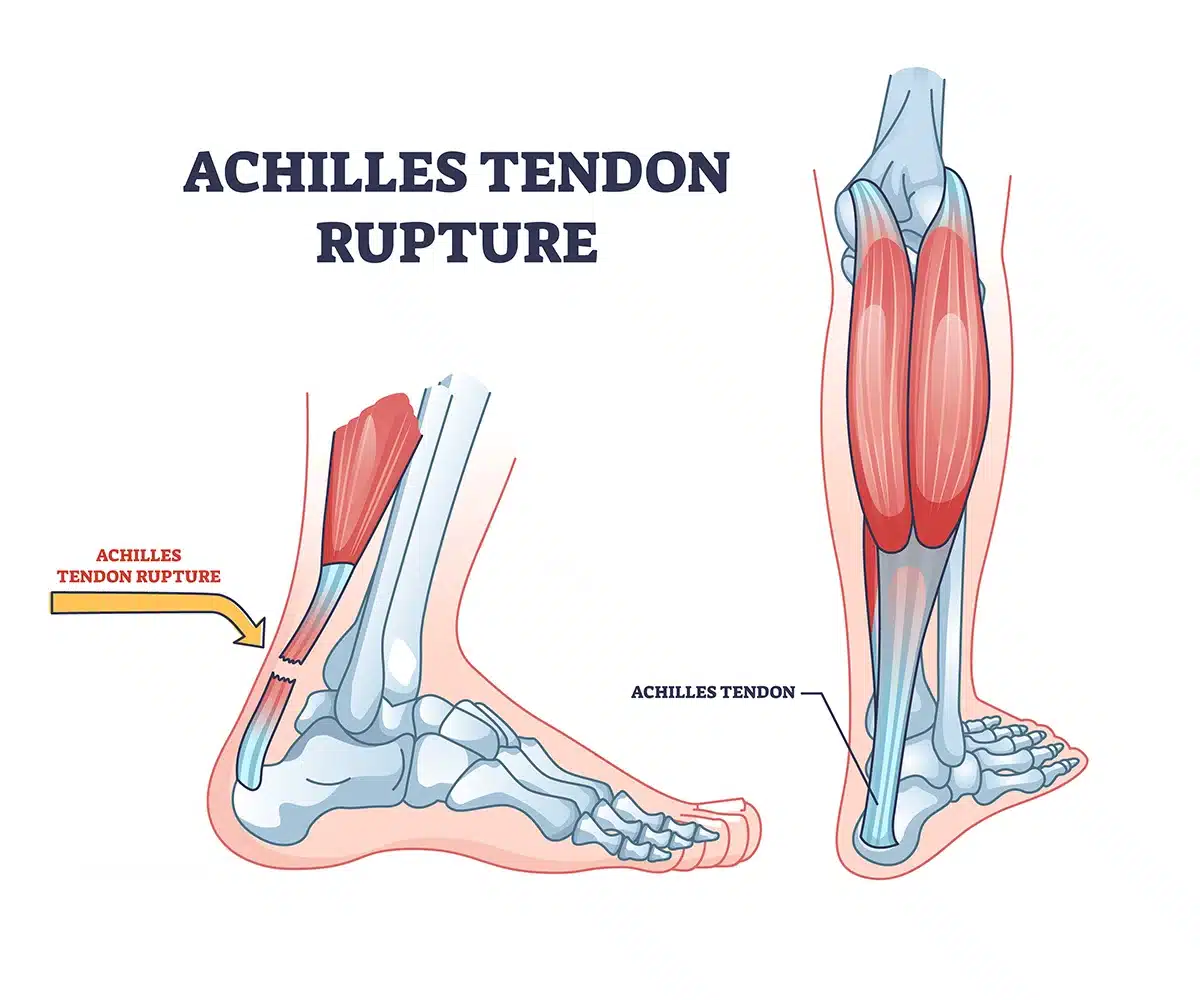
With a rupture, the tear through your Achilles tendon can either be a partial or full tear. These tears are the result of your tendon being stretched beyond its breaking point. They’re more common in 30 to 40 year old’s, and more so for men than women.
Symptoms
The classic telltale sign that you’ve ruptured your Achilles tendon is feeling (and maybe even hearing) a snap or pop at the back of your ankle. It actually can be such a distinct incident that often people mistakenly think they’ve been hit in the ankle by something, when in fact it’s just their tendon snapping.
As you can imagine, rupturing a tendon is extremely painful. Most people describe almost immediately feeling a sudden sharp pain near their ankle. Getting bruising or swelling is normal and nothing to be overly concerned about. Walking is also going to be pretty painful, especially on an incline and going up stairs.
Causes
For the strongest, largest tendon in your body to rupture, there needs to be a pretty strong force. This usually comes in the form of sudden quick movements that stresses your Achilles tendon. Sports with a lot of starting, stopping, and pivoting are often to blame.
You can tear your tendon other ways too. As silly as it sounds, just missing a step on the stairs or accidentally twisting your ankle can cause a rupture. Getting steroid injections near your ankle can also put you at a higher risk because it weakens your Achilles tendon.
Diagnosing
Rupturing your Achilles tendon is a pretty traumatic injury, so you should seek medical attention right away. If you don’t, it might not heal properly, which would just increase your odds of it rupturing again in the future.
When your doctor is doing the exam, they’ll look closely at your ankle and foot. They’ll move them in different directions and press gently on the area to see how it reacts. They’ll also see if they can feel a gap in the tendon where the tear would be. You could be sent to get an MRI or ultrasound to help confirm the size of the tear.
Treatment
Most doctors typically recommend surgery to repair a torn tendon. This is especially true if you’re middle aged (or younger) and are fairly active. The surgery itself is simple, and you’ll be able to regain full function of your Achilles tendon after you’re done healing.
Whether you go the surgical route or not, you’ll want to make sure to start physical therapy sooner rather than later. At PT, you’ll work one on one with the therapist to get your mobility and strength back to how it used to be. It usually takes around 4 to 6 months for a torn Achilles tendon to fully heal. During that time, your physical therapist will help ensure you don’t do anything that your body isn’t ready for, so you don’t end up prolonging your recovery.
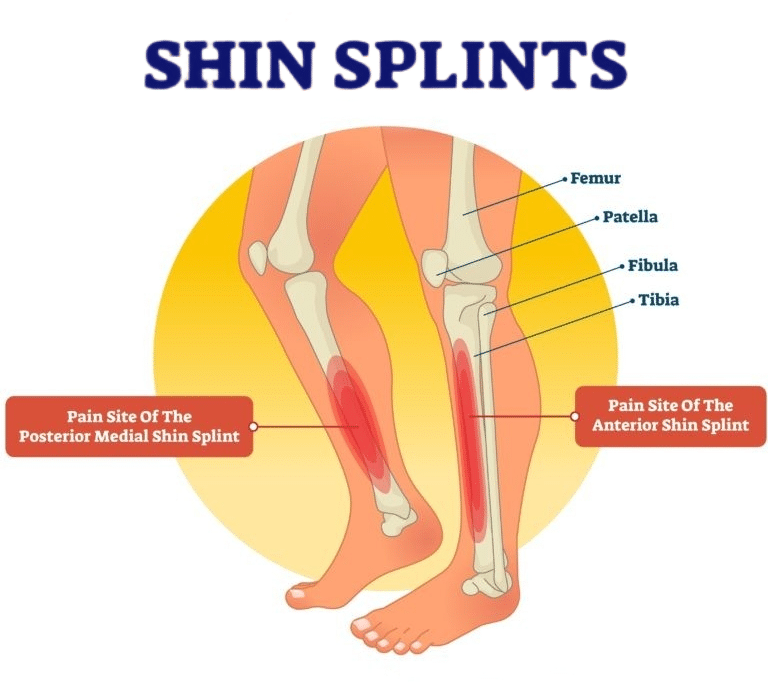
Shin Splints
Shin splints are another type of muscle injury you may experience. It’s characterized by inflammation in the muscles and tendons around your shin bone (tibia.) While your shin is technically considered part of your lower leg, the muscle affected by shin splints runs all the way down your foot into your big toe. That muscle, called tibialis anterior, is what allows you to lift your foot and your toes. Doctors sometimes refer to shin splints as medial tibial stress syndrome (for obvious reasons.)
Symptoms
If there’s one thing that shin splints are known for, it’s pain. Most people feel it in the front of their shin or inner part of their lower leg. It’s common for the pain to come and go in the beginning, especially when you’re being active. After a while, it tends to progress into a persistent steady pain, even after you’ve finished your activity. What originally started as a dull ache can quickly turn into a sharp throbbing sensation. You might also notice some swelling too, which will likely be tender to the touch.
Causes
When you develop shin splints, it means you’ve irritated your shin bone to the point it’s become inflamed and even weakened. This happens when all the muscles and connective tissue in your lower leg repeatedly tug and pull over and over again. When you don’t give your bone a chance to heal, that’s when the damage can get worse.
Anyone can get shin splints, but there’s certain people who are more likely to develop it. Since it’s an overuse injury, it’s common in runners and athletes playing high impact sports. People who walk a lot or are on their feet for work are prone to them too.
Believe it or not, you may have to blame your feet for your shin splints. If you have flat feet or very rigid arches, your muscles aren’t able to distribute the force from impact, which ends up stressing your shins. The same principle applies when you exercise in shoes that don’t offer any support.
Diagnosing
In order to diagnose shin splints, your doctor will need to do a complete physical exam. They’ll check out your lower leg, ankle and foot, then move them around while looking for any sort of tenderness along the bone.
If standing or hopping on your leg is painful, that could indicate shin splints or possibly stress fractures, which are tiny cracks in your bone. Shin splints can progress into a stress fracture if you don’t let your leg heal. Your doctor will order an MRI or X-rays if they need to rule out stress fractures.
Treatment
The best thing you can do when you get shin splints is take the pressure off of your bones and muscles so they can begin to heal. Most people can make a full recovery without any long term problems, as long as you don’t put off treatment. That’s why it’s a great idea to start physical therapy early on.
Now, you’re probably wondering how physical therapy can help. At physical therapy, you’ll learn how to move safely without putting more stress on your shins (which would just make your injury worse.) At first, you’ll work to strengthen your legs through a specialized exercise program. The stronger you can make your muscles, the more they can support you and protect you from reinjuring yourself.
As you progress and get stronger, you’ll be able to slowly increase your activity level. Your therapist will incorporate different types of exercises and activities that will challenge your body. This is one of the most necessary parts of recovery because it allows you to work towards returning to your normal activities without making your condition worse.
Sesamoiditis
This next injury is pretty unique. It’s called sesamoiditis and it occurs when your sesamoids become inflamed. Sesamoids are these 2 little bones that are actually embedded into the tendons of your foot, right below the joint of your big toe. Think of it like an enhanced version of tendinitis, where both the tendon and the tiny bones inside of them are inflamed.
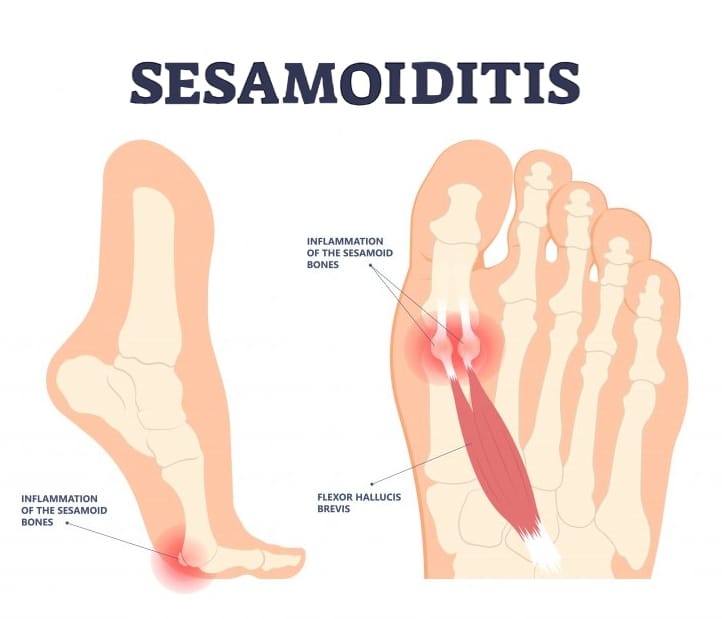
Symptoms
You may notice a few different symptoms with sesamoiditis. For one, you’re bound to have pain in the ball of your foot, which isn’t very surprising since that’s where the tendon (and both bones) are located. You might not be able to put much weight on it either. All the inflammation can also make it difficult to bend your toe.
Typically, sesamoiditis develops slowly over time, so you might not realize where your symptoms are coming from right away. It might start off like a dull ache near your big toe. Then, some swelling and possibly tenderness when you touch your toe. After a while, that pain can become more of a sharp, throbbing sensation.
More than likely, it’ll be the timing of your symptoms that tips you off that you have sesamoiditis. In the beginning, you might not notice anything until you start using your foot. And once you stop, it could all go away. Eventually, the pain, swelling, trouble walking- everything- will become so persistent that it’s very obvious something serious is going on.
Causes
Most foot injuries are caused by overuse or repetitive strain, and sesamoiditis is no different. When you go onto the balls of your feet, your tendons have to flex so they can hold your weight and move in different ways. As for the big toe side of things, those tendons have to glide over the sesamoid bones to use as leverage.
So, whenever you do any type of activities or movements that places you on the balls of your feet, you directly strain your tendons and bones. And if you’re continuously doing this, it can end up causing sesamoiditis and potentially even a stress fracture or two. This is typically a frequent issue for athletes or anyone that tends to wear high heels often.
Diagnosing
In order to diagnose sesamoiditis, your doctor will have to exam your foot, especially the big toe area. They’ll look for signs of inflammation and tenderness near the sesamoid bones. Then, they’ll move your toe (gently, of course) in different directions to see if it causes pain. They might even do something called a passive axial compression test where they move your joint in a way that simulates the way you walk.
Treatment
Luckily, treating sesamoiditis is fairly simple. Initially, it’ll consist of resting your foot. After a day or so, you’ll want to take a more hands on approach. The trick is finding ways to keep up your mobility without stressing the injured part of your foot. Can you guess who happens to be experts in these kinds of situations? Physical therapists.
When you start PT, the therapist will create an exercise program unique to you and your injury. These exercises will help you restore your range of motion without hindering your recovery. They may look simple, but they’re designed to work specific muscle groups in a safe and effective way.
The physical therapist will also teach you how to modify risky movements that you may have to do throughout your day. Of course, there are times when you just can’t avoid being on your feet, whether it’s for work or taking care of your family. At PT, you’ll learn ways to protect your foot and actually give yourself a chance to repair the damage. Mild cases of sesamoiditis usually start to improve fairly quickly, while more severe ones can take a few months to completely heal.
The tough part though is going to be getting back to the activities that caused your sesamoiditis in the first place. It’s important to follow your therapist’s guidance so you don’t cause any permanent damage. It might be wise to invest in a quality orthotic to relieve some of the pressure as you gradually work your way back. Sesamoiditis can always come back, so the more you can prepare yourself, the better.
Ligaments
Now that we’ve covered muscles and tendons, let’s move on to ligaments. There are dozens of ligaments in your feet, all with different jobs and responsibilities. These strong bands of tissue connect your bones together in order to support your arches and keep your foot stable.
One of the things that can happen to your ligaments is they can get stretched out and tear. When they do, it’s considered a sprain and is extremely common. There are a few different types of ankle sprains, so we’ll start from the top and work our way down.
High Ankle Sprain
The first type of sprain is a high ankle sprain. Your ankle bone, called the talus, connects your leg bones to the rest of your foot. It sits inside a socket formed by the lower part of your shinbone (tibia) and calf bone (fibula). A high ankle sprain is when you damage the ligaments just above the talus that connect your tibia and fibula together.
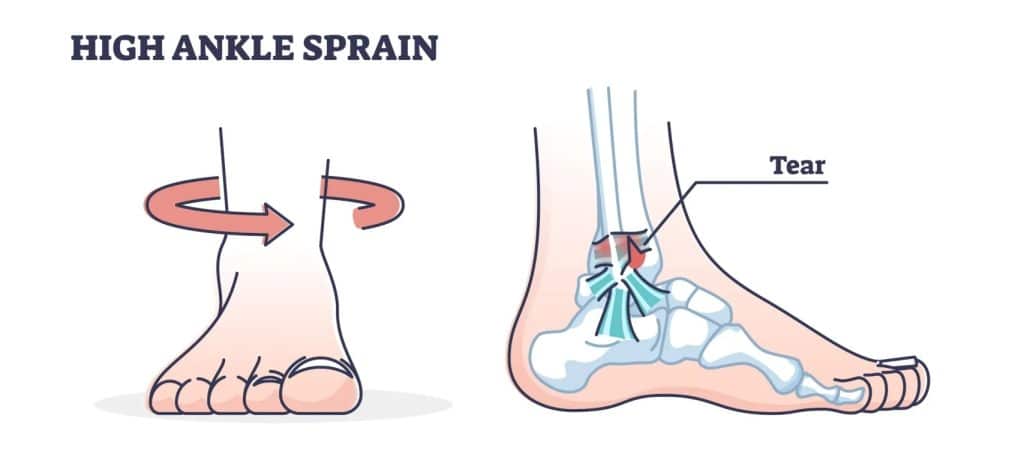
Ankle sprains are divided into 3 different grades, based on the amount of ligament damage.
- Grade 1 sprains are generally mild. Your ligaments only stretched slightly but there could be a very small tear. You’ll notice a little swelling and that your ankle is tender when you touch it.
- Grade 2 sprains are considered moderate. You’re dealing with a partial tear in your ligament at this point. There’s also more swelling around your ankle and it’s quite painful when you move.
- Grade 3 sprains are the most severe. You’ve got a full tear through your ligament now. Your ankle will be completely swollen and you won’t be able to walk or put weight on it.
Symptoms
Ankle sprains are pretty standard when it comes to symptoms. Almost always, there’s some decent swelling that happens. In the case of high ankle sprains, it’s higher up on your ankle, and is usually accompanied by bruising a few days later.
You’ll notice that it’s pretty difficult to use these ligaments when they’re sprained. Putting weight on your foot will be especially challenging, which means things like climbing up a set of stairs is nearly impossible. You also won’t be able to do anything that involves walking on your tip toes either.
Causes
High ankle sprains happen when your ankle turns either inward or outward while your foot is flexed up. Since your foot has to be in that flexed position for this injury to happen, there’s usually a collision to blame. This doesn’t necessarily have to be a collision in the traditional sense (like running straight into someone), but more so some sort of forceful impact like when your foot hits the ground while running or jumping.
Diagnosing
If you suspect you have a high ankle sprain, then you should schedule an appointment with your doctor. There’s a few ways they can test your ankle to make their diagnosis. First, they’ll have you sit on the edge of the exam table with your leg hanging down. They’ll push your foot upward while slightly twisting it to the outside. If there’s a ton of pain while they’re doing this, then it’s very likely you have a high ankle sprain.
Another way to check for a sprain is by doing something called a squeeze test. Like the name suggests, your doctor will squeeze your shin bone and calf bone together. This puts pressure on the ligaments and membrane that separates the two bones. If you feel pain in your upper ankle when they do this, then you probably have a high ankle sprain.
Depending on how clear cut your injury is, the doctor may send you to get some imaging done as well. This can include X-rays, MRI’s, CT scans and occasionally an ultrasound. MRI’s are usually your best bet for ankle sprains, but X-rays can help rule out any other suspected injuries.
Treatment
For the first few days after a high ankle sprain, you should follow the RICE method of rest, ice, compression, and elevation. After that, your doctor will want you to start physical therapy so you don’t lose all of your strength and flexibility. Plus, once you sprain your ankle, you’re more likely to do it again at some point, but PT can help you reduce your chances.
Treatment will be pretty simple in the beginning, with some gentle stretches, sometimes with therapeutic resistance bands. As your pain and swelling go down, you’ll be able to do more at your therapy sessions. Your PT will teach you exercises that focus on making the ligaments around your ankle joint stronger and more flexible.
Another thing you’ll work on at physical therapy is your proprioception. Proprioception is just a fancy term to describe your perception of how your body is moving or positioned. Think of it as body awareness. Kind of like how your body instinctually knows how sit up straight or how to move in order to pick up a pencil. It’s often referred to as our sixth sense and it plays a huge part in your ability to balance. So, your therapist will start to introduce exercises that challenge this mind-body connection to help improve your balance.
Luckily, most people don’t need surgery for this kind of ankle injury, unless there’s severe damage and you can’t regain your stability. On average, it takes around 6 to 8 weeks to recover from a high ankle sprain. It may take a little bit longer for you to return to some of your more physical activities. Your therapist can help you safely work your way back to them though.
Inversion Sprain
The next type of sprain is an inversion sprain. Inversion sprains happen when your ankle rolls outward, which damages the ligaments on the outside of your ankle. When it’s the opposite, where your ankle rolls inward and damages your inside ligaments, they’re called eversion sprains, but those are far less common.
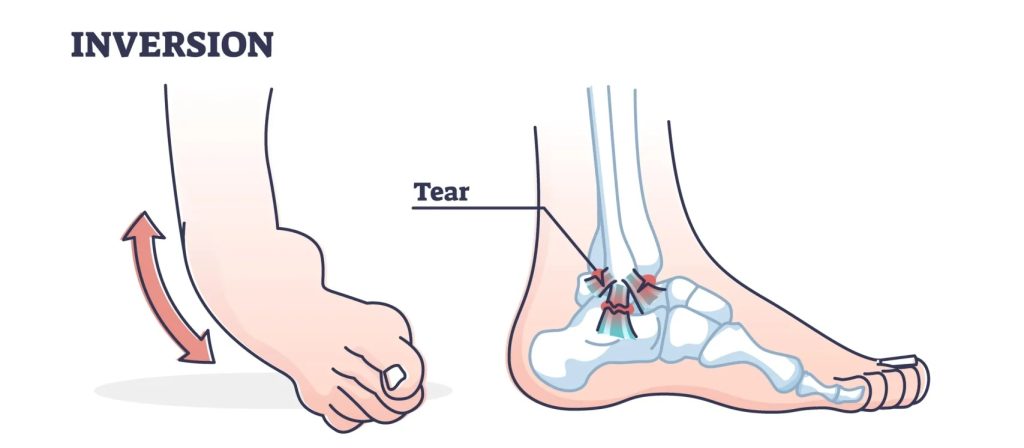
Symptoms
The first symptom you’ll notice with an inversion sprain is the pain. There’s no mistaking that sudden sharp zing you get on the outside of your ankle when it happens. Even while resting, it’s there, but when you try putting weight on your ankle, that pain goes through the roof.
There’s almost always at least some degree of swelling and bruising with inversion sprains. The outside of your ankle will start getting bigger and filling with fluid within the first 24 hours. Then, blue and purple hues develop, followed by a nice yellow green combo.
And since you’ve stretched (and maybe even tore) your ligament, it physically can’t support your foot like it’s supposed to. This leaves you feeling like your ankle is unsteady or about to give out. It can also affect how your foot functions. You might find it difficult to move your ankle with such a limited range of motion. It makes walking pretty challenging too.
Causes
Anyone, no matter their age, can sprain their ankle. Inversion sprains are usually the result of falling or tripping, especially on uneven surfaces. These types of situations make it very easy to twist and roll your ankle. That’s not the only way though. If you lose your balance or land on your foot wrong coming down from a jump, you could overstress your ligaments. This can even happen just by wearing the wrong pair of shoes or jamming your foot by accident.
Beyond your normal everyday stuff, doing any kind of physical activity that has cutting, jumping or kicking involved can really increase your risk of an ankle sprain. This can be anything from playing tennis, shooting hoops with the grandkids, or running on different kinds of terrain while playing tag.
As crazy as it sounds, an already sprained ankle can cause another sprain, but in your other foot. When there’s an inversion sprain, people typically start to walk a bit unevenly. And whether you mean to or not, you end up putting more weight on your healthy foot as a result. This extra stress changes how your ankle functions and makes it more vulnerable to injury.
Diagnosing
Your doctor can diagnose an inversion sprain by doing a physical exam. They’ll want to take a look at your foot and ankle to check your range of motion and see which ligaments are affected. While your movement will be a lot more restricted during the first few days from all the swelling, it’s usually a big indication that there’s a sprain, even if it’s just a lower grade one.
After your exam, the doctor should do some imaging, like an X-ray or MRI. Luckily, these tests can see through any swelling and bruising going on. They’ll help give your doctor a better idea of your diagnosis so they can recommend the best course of treatment for you.
Treatment
Instead of the RICE method, you’ll want to do the PRICE method with your inversion sprain. It’s still the standard rest, ice, compression, and elevation that you’re used to, but with an added step for “P” (which stands for protection.) Basically, it means using crutches or wearing a brace to help protect your ankle and limit how much you can use it. This also helps when you’re in public because it lets people know to be more careful when you’re nearby.
It’s highly recommended that you sign up for physical therapy once your doctor makes their diagnosis. You’ll be slightly limited with your crutches or brace in the beginning, but it won’t prevent you from making progress. That’s the beauty of physical therapy, even if you aren’t weight bearing, there’s so many things you still can do.
The overall goal for physical therapy is to regain your strength and mobility without making your injury worse. If you don’t let your ligaments heal, they can stay chronically unstable, which means repeat ankle sprains are in your future. On the same side of that coin, if you don’t strengthen your ankle, the injured ligament can get even weaker and put you at risk for more sprains as well.
When you start physical therapy, you’ll work on strength training the tendons and muscles in your legs. The therapist will help you with motion controlled movements without any sort of resistance, then work your way up to using resistance bands. You’ll also do some balance training, which is the best way to prepare you to return to your regular activities. Depending on the severity of your sprain, it can take anywhere from 6 to 12 weeks to fully heal.
Plantar Fasciitis
Next, is somewhere that’s no stranger to injury: the bottom of your foot. One of the most common conditions that affects this area is plantar fasciitis. Plantar fasciitis is simply inflammation of the fibrous attachment known as your plantar fascia. Think of your plantar fascia like a ligament, but stretchier like a rubber band. It runs all the way from your heel to the ball of your foot, forming your arch.
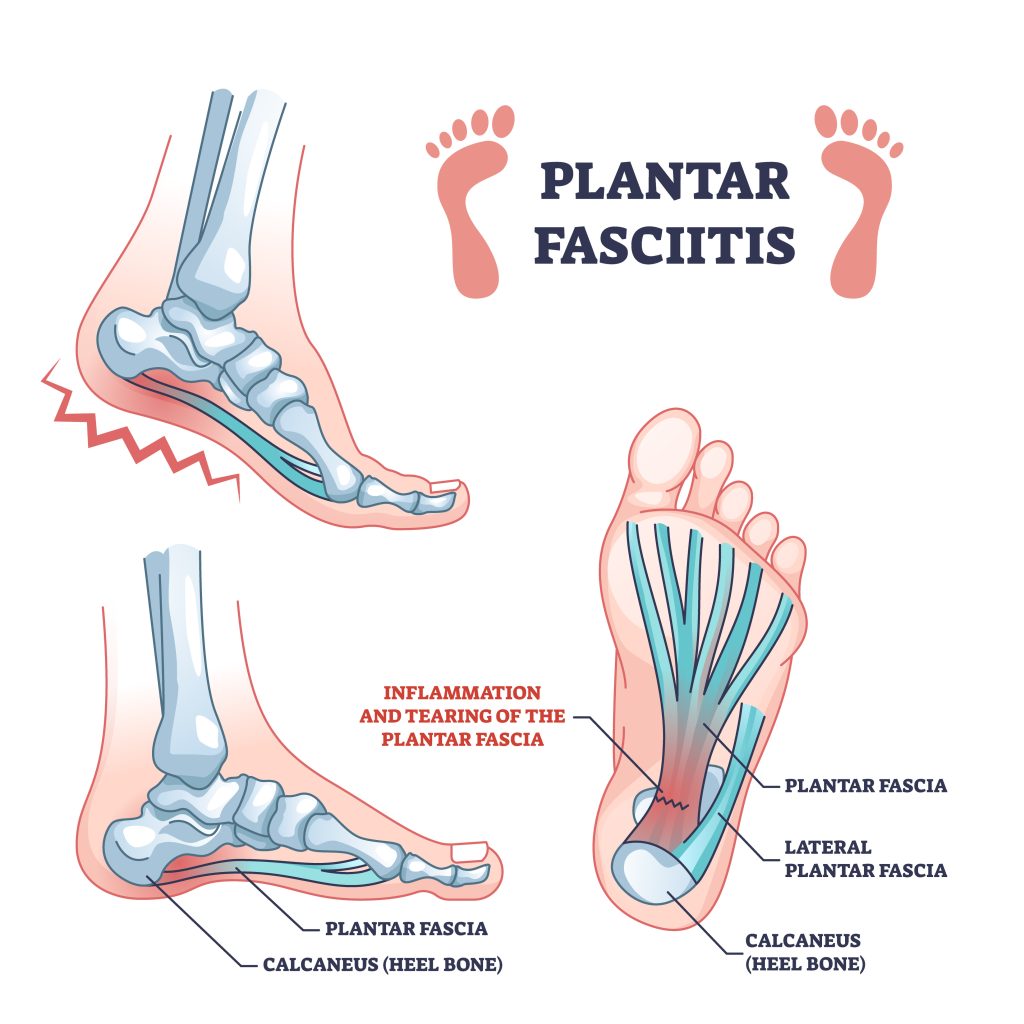
When your plantar fascia is overstretched or overused, that’s when plantar fasciitis happens. Basically, anything that damages your plantar fascia can cause swelling. All of this inflammation makes it painful to use your foot and walk. It’s possible to get plantar fasciitis in both of your feet at once, but it usually pops up in one foot at a time.
Symptoms
Saying that plantar fasciitis is common is an understatement. Around 1 in 10 people will get it at some point in their life. That means more than 2 million people need treatment every year.
The main symptom of plantar fasciitis is pain. Pain in your heel, pain in the arch of your foot, pain in both spots at the same time. It could feel like a dull, constant ache or sharp and stabbing when you put pressure on your heel.
The pain can also change depending on the time of the day or what you’re doing. For instance, you’ll probably notice more pain when you first stand up in the morning or after you’ve been sitting for a while. Luckily, it tends to go away after walking around for a few minutes. It might seem counterintuitive, but sometimes exercising can temporarily relieve your pain, but then get worse as soon as you’re done.
Since plantar fasciitis is all about inflammation, it’s not surprising that most people get swelling around the heel of their foot. This swelling makes it difficult for your plantar fascia to move like it should, which is why you’ll notice some stiffness. It can also cause your Achilles tendon to tighten up in response too.
Causes
Basically anything that damages or irritates your plantar fascia can cause you to get plantar fasciitis. Playing sports is typically a big one, but something as simple as exercising without warming up or stretching can do it too.
You don’t even have to be an athlete either. If you’re someone who has to be on their feet all day or have to work on a hard surface like a sidewalk or warehouse floor, then you’re just as likely to develop plantar fasciitis.
Some things you might be doing at home may also be the culprit. Standing and walking around barefoot is one of the leading causes. Wearing shoes that aren’t supporting your feet is almost just as bad. Think along the lines of flip flops or sneakers that you can easily bend and twist- they’re not doing you any favors.
Diagnosing
Even if the signs are all there, your doctor will need to do an exam to diagnose plantar fasciitis. They’ll talk to you about the types of symptoms you’re experiencing and when they seem to get better or worse. Then they’ll take a closer look at your foot. Usually, this involves pressing lightly on your plantar fascia and heel to feel for any inflammation and see what your pain level is at for those areas.
Treatment
The good news is, most people recover from plantar fasciitis without needing any sort of invasive treatment. What’s shown to be the most successful is combining a bit of rest with physical therapy (and occasionally some pain meds in the beginning when your foot is still pretty tender.)
One of the best things your physical therapist will do is show you safe and gentle ways to stretch the arch of your foot and your Achilles tendon. You don’t want to avoid moving them altogether, to the point that they lock up and lose flexibility. You also don’t want to overdo it and cause more stress and inflammation either. The key is in the middle and your physical therapist will help you find that balance.
Physical therapy is also where you’ll work to strengthen your ankle and lower leg. The stronger your muscles and ligaments are in those areas, the more stability they can provide. Finding the right exercises can be challenging, especially ones for your feet, which is why PT is so beneficial. Everything you learn inside the clinic you can do at home too, so you’re always working toward being able to do the things you love again.
Morton’s Neuroma
This next injury isn’t talked about quite as much as something like plantar fasciitis or Achilles tendinitis, but it’s still surprisingly common. So common, in fact, that 1 in 3 people get it at some point in their life. It’s called Morton’s Neuroma and it involves inflammation of a specific nerve in your foot.
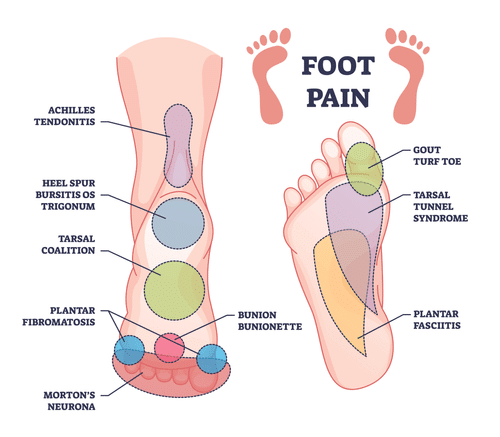
The nerve in question connects your third and fourth toes together (kind of like your “middle” toe and “ring” toe, so to speak.) You can find that area highlighted red in the picture above. When you have a Morton’s neuroma, that nerve is thick and swollen.
The term “neuroma” is slightly misleading in this situation because typically neuromas are referring to noncancerous tumors that form on nerves throughout your body. Morton’s neuroma, however, isn’t new tissue that’s growing on one of the nerves in your foot. It’s not a tumor at all, really. It’s also not a symptom of cancer and doesn’t cause cancer. What it actually is, is just one of your existing nerves that’s become inflamed.
Symptoms
The most common symptom with Morton’s neuroma is pain between your 2 toes, especially when you’re walking or standing. Think of it like having a pebble in your shoe or stepping on a Lego (which is the absolute worst!) It feels sharp and maybe even a little stingy. Wearing high heels and being on the balls of your feet make it even more painful. There’s usually some numbness and swelling too. You might get the feeling like you’re walking on pins and needles too.
Typically, all of these symptoms get worse over time. You may notice only a bit of pain in the beginning, but once you take your shoes off it goes away. As you get more and more inflammation on that nerve, everything will be a lot more heightened and obvious.
Causes
Experts aren’t exactly sure what causes the nerves between your third and fourth toe to swell. They think it’s likely from putting pressure on that nerve and the ball of your foot though. There does seem to be a link between certain health conditions and the odds of developing a Morton’s neuroma. This includes things like high arches or flat feet, hammertoes, and bunions.
Certain activities can also increase your risk. Wearing high heels or even just shoes that have a narrow, pointed toe area are big ones. Sports that put you on the balls of your feet a lot, like running, tennis, or pickleball, can cause it too. The same goes for an activity or job that requires you to be on your feet all day.
Diagnosing
When it comes to diagnosing a Morton’s neuroma, your doctor can usually do it just by examining your foot. Make sure you call them right when you notice any symptoms so you don’t end up causing nerve damage or any other complications.
During their exam, the doctor will put some light pressure in that area between your 2 toes to see if they notice any swelling. They may ask you to stand, walk, or move around so they can observe your foot in action. They’ll also want to know when you initially noticed any symptoms and what positions or activities make them worse. If they suspect other nerve conditions that have similar symptoms, they can always send you to get imaging tests done.
Treatment
If you’re like most people, then you won’t need to get surgery for your Morton’s neuroma. You don’t want to ignore it hoping it will go away either. The best thing you can do is use treatments that relieve your symptoms and work to protect the area around your affected nerve. You can easily do this through physical therapy, where you’ll learn various exercises that focus on improving your strength and flexibility.
Once your pain and swelling has gone down, you should be ready to start trying some of your normal activities again. It’s important that you don’t just rush and jump back into them without having your physical therapist evaluate everything first. The PT will look to see if there’s any risky movements or positions involved and figure out ways to make them safer until you’re fully healed. This could be something as simple as wearing different shoes at work or modify the way you crouch down on the ground.
Bones
Now, it’s time to look at your bones. There are 26 bones in your foot, which are grouped into tarsals, metatarsals, and phalanges. The way they line up naturally divides your foot into the 3 different sections: the hindfoot, midfoot, and forefoot.
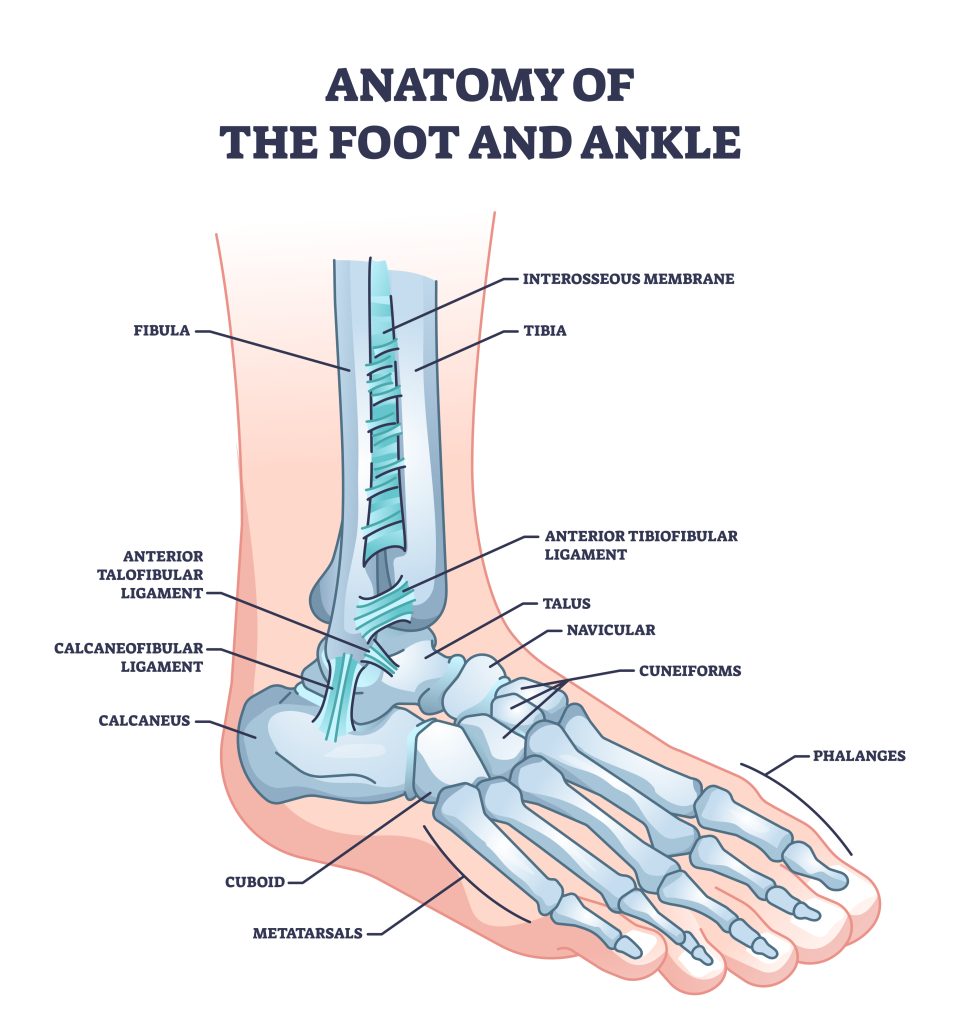
The hindfoot forms your ankle and heel. It’s made up of the talus bone and the heel bone, known as the calcaneus. Then there’s the midfoot, which is in the middle of the hindfoot and forefoot (hence the name.) There’s a cuboid, navicular, and 3 cuneiform bones within the midfoot. Lastly, the forefoot, which is the front part of your foot. The bones right in front of your midfoot are called metatarsals. They connect to your toe bones, otherwise known as phalanges. Each toe has 3 phalanges, except for your big toe. Your big toe only has 2 phalanges, but also 2 tiny sesamoid bones underneath that forms the ball of your foot.
Jones Fracture
With so many bones in such a small area (that you use all the time,) there’s bound to be injuries at some point. Let’s take a look at the first kind of injury: bone fractures. Fractures are just a fancy way of describing a bone break. The most common is called a Jones fracture, which happens when you break your 5th metatarsal- the bone that connects your pinkie toe to the rest of your foot.
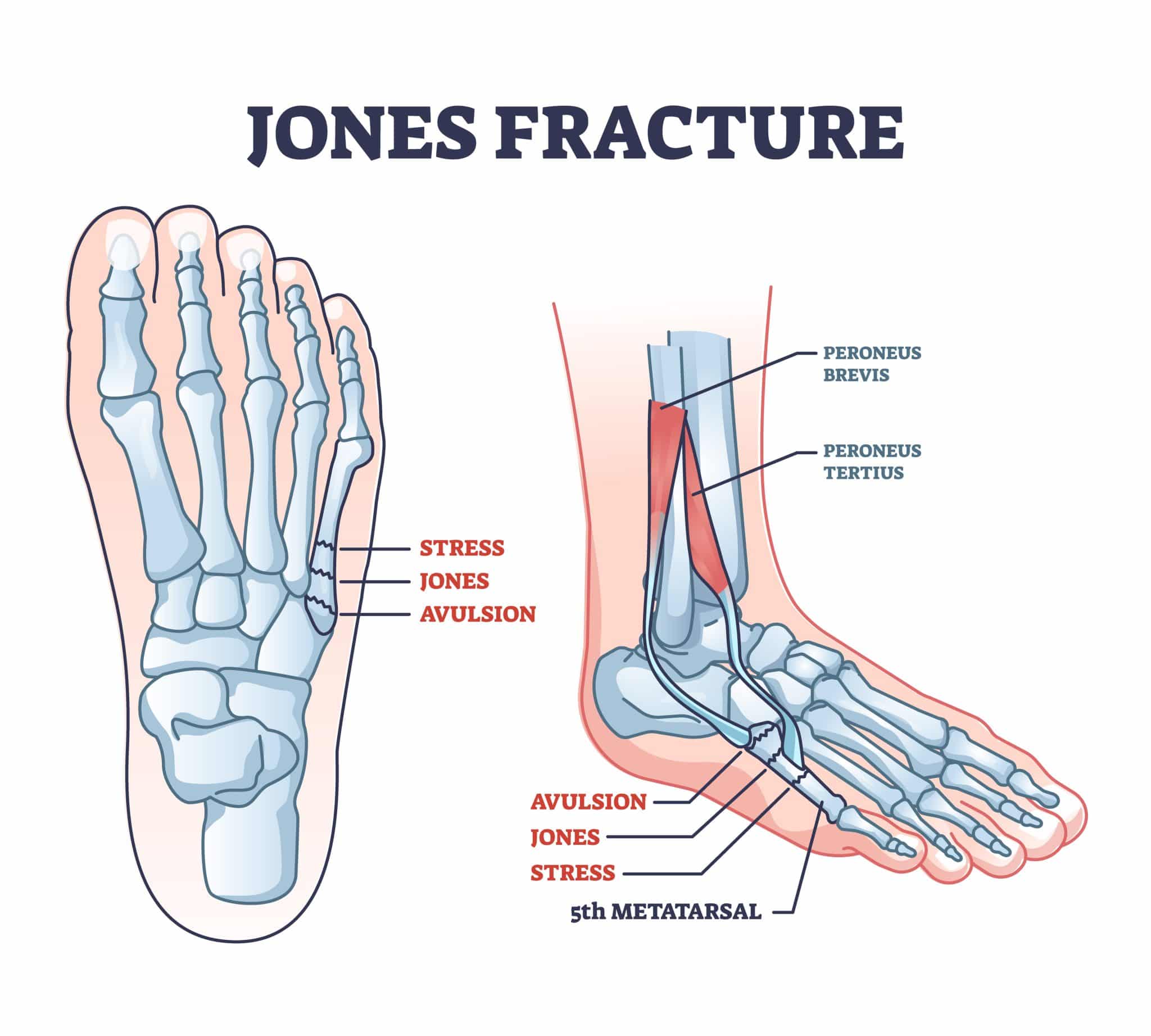
You see, when it comes to your metatarsals, there are 3 different zones where the break can occur.
- Zone 1 is the area near the base of your metatarsal, where it connects to your midfoot. Breaks in this zone can go by a few different names, like avulsion fracture or dancer fracture. Luckily, this kind of break doesn’t require surgery, just a few months in a boot or cast to heal.
- Zone 2 fractures happen in the middle of your metatarsal. This is the zone where Jones fractures happen. You almost always need surgery for a Jones fracture, and they come with a higher risk of complications compared to other foot fractures.
- Zone 3 is the end part of your metatarsal that connects to your toes. Usually, it’s stress fractures that make up zone 3. They can take a bit longer to heal, but don’t always need surgery in order to heal.
All of these names and terms can be a bit confusing, but at the end of the day, they’re all talking about a fracture. For now, back to Jones fractures.
Symptoms
As with any bone break, Jones fractures are typically pretty painful. For the most part, it’s usually localized to the outside of your foot near your pinkie toe. And while there isn’t exactly a ton of “meat and potatoes” (so to speak) in this area, there can still be a good amount of swelling and bruising that can go on.
Depending on your fracture, you’ll likely notice that it’s hard to walk how you normally would. If you have something called a displaced fracture, then the broken pieces of your bone have moved so much that there’s gaps between them. Non-displaced fractures are still considered a break, but the pieces haven’t shifted out of alignment. They’re the least complex of the 2, so your symptoms may not be as severe.
You might find yourself putting more of your weight through the rest of your foot when you’re trying to walk. Whether it’s a conscious decision or not, it’s best to avoid doing this as much as possible because it could actually end up causing stress fractures. More on that in a little bit though…
Causes
Jones fractures are the result of a sudden force or impact to the outside of your foot while it’s twisted away from your body. Usually, this comes in the form of repeated overuse, like standing or walking on hard surfaces for too long. It might also happen if you trip on the stairs or catch yourself after slipping on ice.
Like most fractures, Jones fractures can affect anyone, but are more common for men in their 30’s and women over 70. They’re also more prominent for anyone who puts a lot of stress on their feet, like athletes or workers that stand or walk most of their shift. Having health conditions that weaken your bones, like with osteoporosis, can increase your likelihood for all types of breaks, Jones fractures included.
Diagnosing
In order to diagnose a Jones fracture, your doctor will need to do an exam followed by imaging tests. Most times, a simple X-ray will confirm the break and show just how much damage (and possibly displacement) your bones have sustained. If the doctor is worried about complications or additional injuries, they may also do an MRI or CT scan to get a better idea of what’s going on.
Treatment
As for treatment, it’ll come down to the severity of your fracture. If your bones moved, you’ll need to get them realigned through a procedure called a closed reduction. If your fracture is more mild and things have stayed in place, then you may only need a boot or cast for a couple of months.
Once you get the cast or boot off, you want to start physical therapy as soon as you can. You might not be able to put much weight on your foot in the beginning, especially if you’re coming off of a surgery. Gradually, you’ll be able to handle more and more though.
The main thing you’ll focus on is getting the strength and range of motion back in your foot. Luckily, you should expect a full recovery from your Jones fracture. Most people take around 3 to 4 months before they’re back to doing their normal activities, even playing sports.
Stress Fracture
Next, stress fractures. A stress fracture is a small crack in one of your bones after being put under too much stress, exactly as the name suggests. Sometimes they’re referred to as hairline fractures since the tiny break in the bone resembles a thin piece of hair.
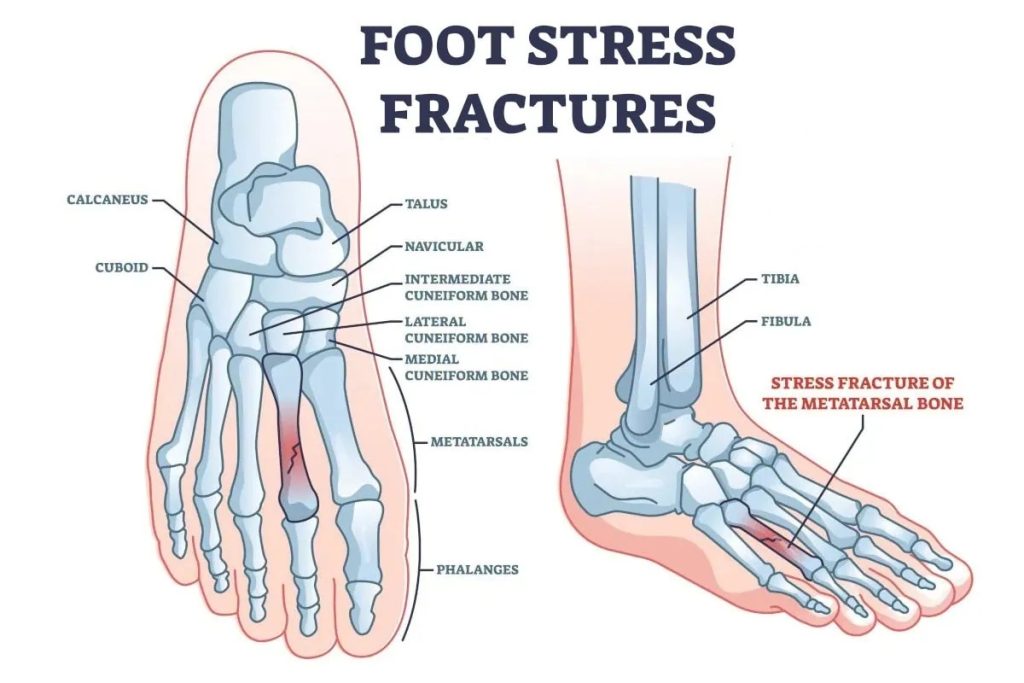
Of all the body parts, your feet are the ones known for stress fractures. That’s because stress fractures heavily affect weight bearing bones. The bones in your feet are what supports your weight anytime you’re standing or moving, which means they’re constantly under a ton of stress. Most of the time, it’s your metatarsals that take the brunt of everything, but occasionally your heels (calcaneus) can too.
Symptoms
When there’s a stress fracture in your foot, the first thing you’ll feel is the pain. Unfortunately, once it starts, it usually doesn’t stop. It’ll get worse when you’re up and moving around, but it’ll still be there when you stop. After a while, it’ll become more obvious when you’re just resting.
The bulk of your symptoms will probably stay localized to the area near where the fracture is. So, if you fracture your 5th metatarsal, your entire foot might be in pain, but the spot near your pinkie toe will hurt the most. That’s where you’ll find the majority of your swelling as well.
Causes
Stress fractures are pretty much always caused by an overuse injury. They start out as inflammation on the surface of your bone. Doctors tend to call this a stress reaction, which is like a deep bone bruise. If you keep putting pressure on that spot before it can heal, the bruise will reach deeper down into the bone until it starts to crack and becomes a stress fracture. They develop when you have to do repetitive motions, usually while training for a sport or during work.
Nearly 20% of all sports injuries are stress fractures. Maybe you trained too much without enough rest or didn’t use the right equipment. Or you started a new type of workout or increased your activity level too quickly. All of these can lead to stress fractures. The same goes for training (or working) on a different surface that you’re not used to. It may not seem like much, but simple things like switching from an indoor track to outdoor road or starting a new job where you stand on concrete all day can wreak havoc on your bones.
Even if you aren’t very physically active, there are still some factors that increase your risk of a stress fracture. Being overweight means your bones have to deal with more pressure to support your body. Having high arches or no arches at all (flat feet) also puts added stress on your bones. And of course, any type of health condition that weakens your bones, like osteoporosis or a vitamin D deficiency, makes your odds higher too.
Diagnosing
Getting a physical exam from your doctor is the first step in diagnosing a stress fracture. They may feel around the area or have you stand on your foot to test for pain. But in most cases, they’ll take an X-ray to confirm there is a break and how severe it is.
Treatment
Your initial treatment will depend on the severity of your fracture, like if the pieces of bone have shifted or stayed in place. Most people don’t need surgery to treat their stress fracture, unless they’re having extreme symptoms. Either way, you’ll want to stop physical activity for the time being, especially if it’s the reason for your fracture.
Once you start treating your symptoms and stop putting stress on your foot, you should start feeling better. This is when you’ll want to start physical therapy so the fracture will continue to heal properly. It may be tempting to get back to your normal routines and activities, but it’s important to wait until your therapist gives the OK. Even if you’re feeling better, you need to give your bone time to heal and work on regaining the strength and mobility in your foot. Plus, you can easily make the fracture worse if you try something your body isn’t ready for.
Talus Fracture
The last fracture we’ll go over is a break in your talus bone, called a talus fracture. Your talus is the bone that connects your ankle to your 2 lower leg bones, the tibia and fibula. Together, they form your ankle joint, which allows you to move your foot up and down. The talus also sits above your heel bone, forming the subtalar joint. This is the joint that lets you move your foot side to side.
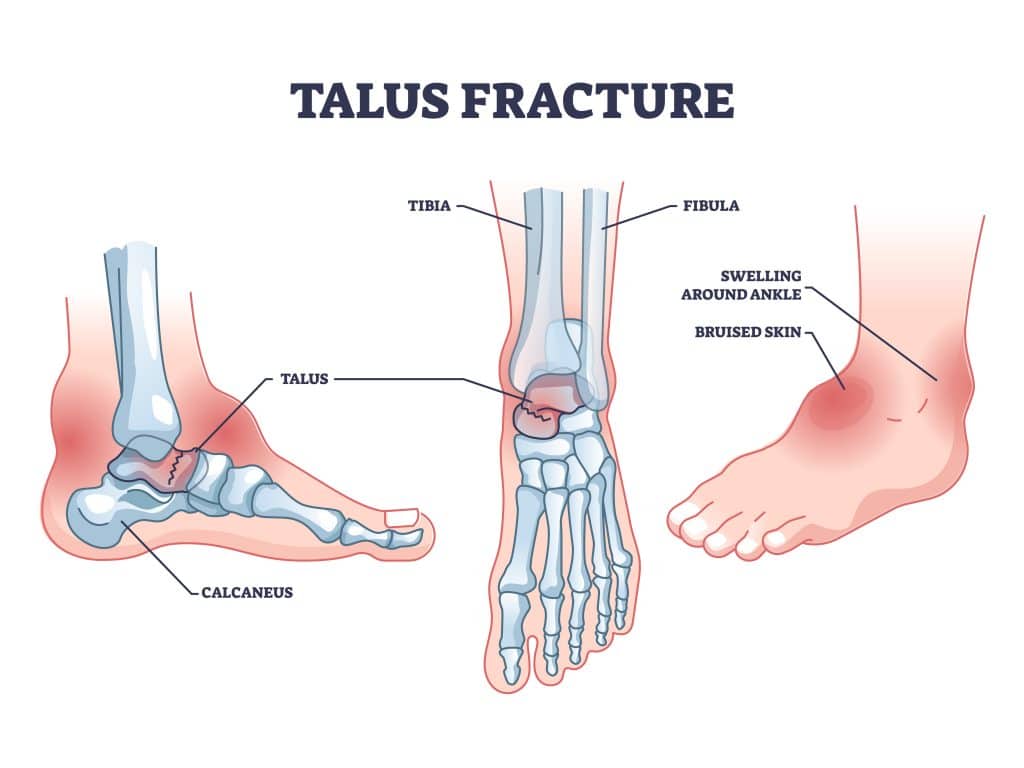
Your talus is mostly covered in cartilage and is responsible for transferring weight across your ankle. Normally, your bones should be able to move smoothly against one another. But, a fracture to your talus bone can cause a significant loss of function and motion. That’s how important this bone is for your ankle movement.
The talus bone is unique because it can break in different areas and in different ways. A break can happen anywhere along the bone, but the most common spot is in the middle. The outside area (called the lateral process) comes in a close second. Fractures to the lateral process usually happen when your ankle is forced out toward the side.
Types Of Talus Fractures
Your talus bone can go through something called a talar avulsion fracture. This is when a small piece pulls away from the rest of the bone that’s still attached to a tendon or ligament. You can also get a stress fracture in your talus bone as well. Like you probably just read about, this type of fracture happens after repeated stress to your bone causes it to break.
With talus fractures in particular, they’re classified by how much the broken pieces of bone have moved from their usual position. If they are only a bit out of place but still line up correctly (or close to it) then you have a stable fracture. If they’ve moved so much that there’s gaps between the pieces, then it’s a displaced fracture. Now, if your broken talus bone has pierced through your skin, you have a compound fracture.
Symptoms
Most foot fractures have a fairly limited list of symptoms, talus fractures included. Generally, you can count on some severe ankle pain, swelling, and bruising within the first 24-48 hours. Before those fully set in, you’ll probably find it difficult to walk or put any weight on your foot at all. At some point, you may even develop fracture blisters, which are fluid filled blisters on your skin near where the break is.
Causes
Talus fractures are often caused by high impact injuries. These injuries involve a strong force directly to your foot, like a car accident or after a fall from high up off the ground. They’re also a common sports injury, especially for snowboarders. Occasionally, you can get a talus fracture from twisting your ankle, which can actually end with small chips breaking off the edge of your bone.
Diagnosing
If you suspect you broke a bone in your foot, you should see your doctor right away. You’ll want to try to limit putting weight on your foot as much as possible until your appointment. During the exam, your doctor will look for signs of swelling, bruising, and cuts on your foot and around the ankle.
They’ll likely do things like tell you to wiggle your toes, which is a way to see if there’s any nerve damage. Checking the strength of your pulse points lets them know there’s a good blood supply in your foot. One of the most important things they’ll do is make sure you don’t have any fluid building up in the muscles around your ankle and leg. This is a condition called compartment syndrome, and if it’s not treated quickly, you can lose feeling and function in your foot. At the end, they’ll do an X-ray to confirm where the fracture is located and how severe the damage is.
Treatment
As you’ve probably come to imagine, treating a talus fracture will all depend on the type of fracture and how severe it is. In most cases, surgery is recommended since it’s usually a high impact force that caused the injury in the first place, meaning the damage is probably too complex to heal properly on its own.
Even though your talus isn’t exactly the biggest bone, there are actually a lot of complications that can come from it not healing correctly. For starters, you could develop posttraumatic arthritis. Like all bones, the talus is covered in cartilage. So, when you injure your talus, you also injure the cartilage around it too. And when that isn’t smooth and even anymore, your ankle joint starts to go through wear and tear, which can lead to arthritis.
Besides that complication, you also risk going through something called a malunion. Malunions happen when the pieces of your fractured bone don’t heal in their correct position. This can become a permanent issue and make it extremely difficult to walk. On the flip side, if your fracture hasn’t healed after an extended period of time, you have what’s referred to as a nonunion.
Possibly the most severe complication you can encounter is osteonecrosis (or similarly, avascular necrosis.) Basically, when you get a fracture, you run the risk of interrupting the blood supply to that bone. If your talus doesn’t get its needed blood supply, the bone cells start to die and can end with your bone collapsing altogether.
Road To Recovery
With or without surgery for your talus fracture, you’ll have to get a boot or splint to keep your ankle from moving. This will help hold your bones in the right spot while they heal. When you’re able to start walking again, you’ll have to make sure you only put minimal pressure on your foot for about 8 to 12 weeks.
While your talus bone is healing, your doctor will want you to do physical therapy so you can start improving the mobility in your ankle. The physical therapist has exercises and stretches that deal with flexibility all without even needing to put weight on your foot.
They’ll also teach you exercises that strengthen the muscles, ligaments, and tendons around your ankle. Slowly, you’ll be able to put more and more weight on your foot. Then, you’ll be able to shift your focus toward your stability and balance. You’ll work to improve the range of motion and overall function of your ankle so you can return to your normal activities without risking rebreaking your foot.
Bunions (Hallux Valgus)
Now that we’ve covered fractures, let’s move on to a different kind of bone injury: bunions. Bunions, otherwise known as hallux valgus, are just bony bumps that form on the inside edge of your big toes, at the metatarsophalangeal joint.
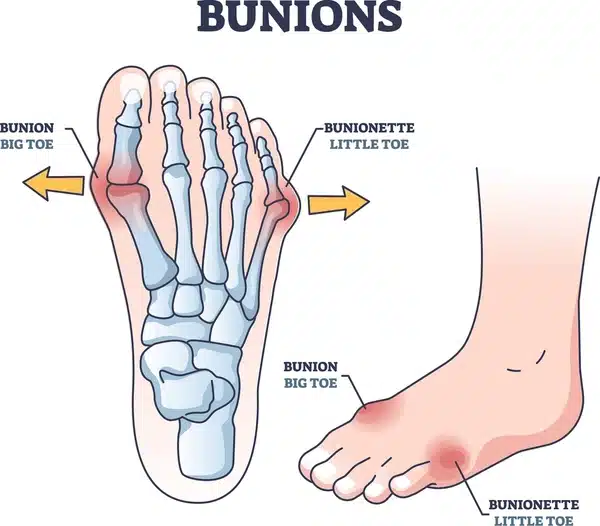
Bunions are an extremely common condition. So much so that nearly 1 in 3 Americans have at least one type of bunion. Standard hallux valgus bunions develop on your big toe from long term pressure. Bunionettes, or Tailor’s bunions, form on your pinky toe rather than the big toe. They’re usually caused because your shoes don’t fit right or you’re doing something that presses your little toe into your other toes.
Symptoms
The biggest tell tale sign of a bunion is the obvious growth that forms on the base of your toe. Not only can you see the bony bump, but you can feel it too. Of course, there are other symptoms that come with it as well. Having that bony bump can make your big toe pretty stiff, to the point where you might not even be able to bend it.
Bunions are also often painful. Bending or moving your toe may cause a burning sensation near the base of it. There can even be some numbness and discoloration around that area too. You might find it difficult to wear some types of shoes, or that wearing them altogether makes your pain worse.
Causes
Unfortunately, there isn’t one single reason to blame for why bunions develop. It’s a combination of factors really, like shoe choice, increased activity, family history, and even the shape of your feet. When there’s extra pressure on the joint of your big toe for an extended period of time- we’re talking years, usually- that added pressure actually pushes your toe out of alignment. Eventually, your body begins to overcompensate for your toe being out of place by forming a bunion.
Now, where that extra pressure comes from, that can be from a few different things. For example, you may walk in a way that naturally puts pressure on that area. Working or standing on your feet too long can do it too. Even something as simple as wearing more narrowed shape shoes, especially near the toe box, will cause enough pressure over time.
While anyone can develop a bunion, they do tend to occur more often in those with a family history of bunions or foot issues. Over 70% of people inherit the condition from a parent who had bunions. There also tends to be a higher occurrence in women than in men.
Diagnosing
Most doctors can diagnose bunions with just a physical exam, but you may wish to visit a podiatrist who specializes in caring for feet. They’ll take a look at your foot and discuss the symptoms you’re experiencing. Try to remember when you first noticed the bump and if there are any activities or movements that can make your symptoms flare up. Generally, you won’t need any other testing than that, but your doctor might do X-rays if they’re worried about the alignment of your bones.
Treatment
If you have a bunion, more than likely you’ll be able to manage your symptoms without many long-term effects to your normal daily living. It’s important that you see your doctor sooner rather than later though, so your condition doesn’t escalate to the point of needing corrective surgery. Most people use a combination of treatments to help relieve their symptoms while keeping their feet strong.
The first thing you’ll want to do is really examine the shoes you wear on a daily basis. If they seem pretty tight, you may want to either try stretching them out or switch to a wider shoe all together. There’s even some over the counter padding you can buy specifically to help take the pressure off of your toes.
Beyond that, it’s a great idea to go to physical therapy so you can work on addressing the root issues with your foot instead of only temporarily masking symptoms. You might think PT is only for back pain or knee replacements, but in truth, it can even help people suffering with bunions.
The beauty of physical therapy is that they’ll look at your body as a whole, and work to improve all the areas that affect your injury, not just the bunion itself. Sure, you’ll get stretches that may help your toe stay in alignment better, but you’ll also learn exercises that strengthen your foot and ankle joint. The more stable your foot is as a whole, the more you won’t have to rely on putting unnecessary pressure on your big toe. Your therapist can also offer advice on the best shoes or orthotics to wear too.
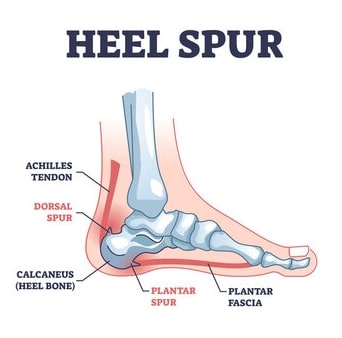
Heel Spurs
This next foot injury affects about 15% of people; it’s called a heel spur. Heel spurs are bony growths on your heel, specifically where your heel bone meets your plantar fascia. They’re made of calcium deposits that have accumulated over time, creating these bony-like protrusions on the bottom of your foot.
Symptoms
Heel spurs are actually kind of sneaky because they develop slowly, so most people don’t realize they have one until they go to the doctor for heel pain. And since they’re located right near your plantar fascia, they often get confused for one another. Plantar fasciitis happens when your plantar fascia gets overstretched or tears. You’ll get an intense stabbing sensation on and off in your heel. Walking helps relieve the pain a bit, but once you sit, it comes right back.
As for heel spurs, they’re actually a reaction to inflammation and stress from plantar fasciitis. What happens is your body responds to that stress by slowly building extra bone tissue, which becomes a heel spur. You would think that an extra bony growth poking out of your heel bone would be quite painful, but a lot of time it goes unnoticed. When it does becomes more apparent, it’s usually described in the same way as plantar fasciitis pain.
Once you know the pain is there, you’ll start to notice some activities really draw it out. The most common include running, walking, and even just standing for an extended period of time. Sometimes the pain may seem sharp in the morning or after you’ve been resting, while it’s more of a dull ache throughout your day.
There’s generally at least some degree of swelling that goes on around the front part of your heel. If you have to be on your feet for work, you’ll likely notice more swelling at the end of the day. Even a little bit of swelling can make walking or anything that involves putting pressure on your heel incredibly difficult.
Causes
As weird as it sounds, growing these heel spurs are just your body’s response to repeated stress on the tendons and ligaments in your foot. This stress can come in the form of overuse, like running or standing on hard surfaces for long periods. If you’re someone with high arches or flat feet, then that uneven weight distribution makes you more prone to developing heel spurs.
Age is also a factor because as you get older, your feet naturally go through more wear and tear. If you’re overweight, carrying around extra pounds puts more of a strain on both your heel and plantar fascia. The same principle applies to wearing shoes that don’t provide enough arch support, increasing your risk of heel spurs.
Diagnosing
Typically when diagnosing heel spurs, your doctor will examine your foot and ask if there was any physical activities that may be the reason behind your heel pain. Ultimately, they’ll want to take X-rays to properly diagnose the heel spurs. This also gives them the ability to rule out plantar fasciitis.
Treatment
Since plantar fasciitis is so similar to heel spurs (and often to blame for causing them), the recommended treatment is the same for both. That’s because treating plantar fasciitis symptoms usually eases any pain associated with having heel spurs.
Unfortunately, surgery is the only way to actually remove a heel spur. Once it’s formed, it’s there for good. It is pretty rare to need surgery though, since most heel spurs don’t usually hurt. And if there is pain, treating the condition that caused the heel spur in the first place should take care of it.
Something you can do right away that will help prevent your injury from getting worse is physical therapy. Similar to plantar fasciitis, you’ll want to start PT fairly quickly after your diagnosis. You’ll learn exercises that strengthen the muscles, ligaments, and tendons that provide stability in your foot. This is especially important because your plantar fascia becomes less flexible as you age, making it more prone to injury.
Modifications
The physical therapist will have a few modifications for you to make as well. For starters, they’ll suggest switching to a supportive shoe, like a running style shoe, even if you’re not going to use them for running. Anything that has a rigid arch that you can’t twist or bend will be beneficial. You can achieve the same thing and turn some of your old shoes infinitely better by investing in a quality orthotic as well.
They may also recommend wearing shoes around your house, especially on the harder surfaces. This can be a controversial topic depending on the household, but it’s an important one nonetheless. After all, home is typically where people spend most of their time. So, it only makes sense to keep your feet supported while you’re standing and walking around inside the house too.
After your therapist becomes familiar with your gait pattern, they might adjust how you walk in order to put less pressure on your heels. They’ll work with you to change different aspects of your daily routine (if possible) so you aren’t on your feet as much too. And the exercise program the PT creates should indirectly help you lose weight, which means less pressure on your foot.
Bursitis
Next, let’s explore bursitis. Bursitis is a general way to describe inflammation of your bursa, which is a fluid filled sac in your joints. And when it becomes inflamed, it causes swelling, pain, and tenderness. In terms of your foot, you can get bursitis in your heel, big toe, side of the foot, and ball of the foot, with the most common being the heel.
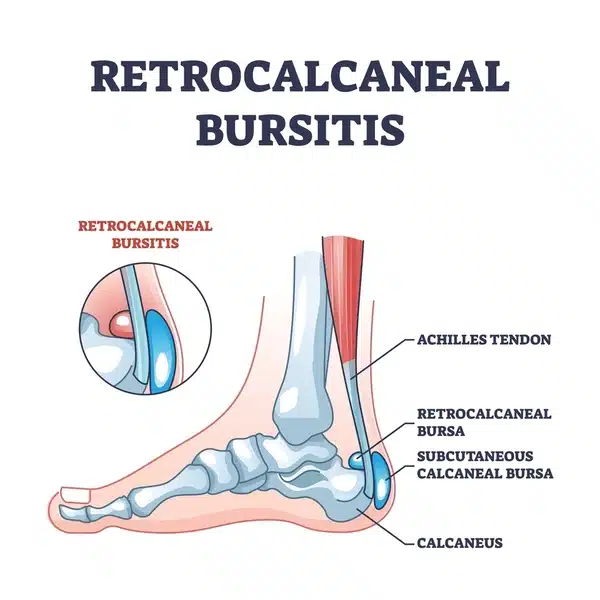
Foot bursitis is rarely discussed compared to muscle, tendon, and ligament injuries, yet it’s surprisingly a very common cause of foot pain. That’s saying a lot since anywhere from 14 to 42% of adults experience foot pain at one time.
Symptoms
If the bursa in your feet are inflamed, you’ll notice a few different symptoms. The first of which is pain and swelling around the affected joint. That swelling and inflammation can really limit how much the joint’s able to move too. There’s often redness around the area as well. It’ll feel warm and tender when you touch it, not to mention painful.
Simple things that were normally easy can quickly become painful when you have foot bursitis. You might notice that walking barefoot or wearing tight socks or shoes makes your pain flare up since it puts pressure on your bursa. Any motions that involve standing on your tiptoes or bending your foot can increase your pain as well.
Causes
There are several different ways you can get foot bursitis. Usually, it’s because of overuse or a traumatic injury. For overuse, it comes down to motions with repetitive impact, like walking on concrete floors all day at work. Traumatic injuries, like a significant fall or car accident, involve direct trauma to your foot, resulting in an injury (in this case, bursitis.)
Any direct pressure on the area above the bursa, like when you wear shoes that are too small, can cause foot bursitis. Certain structural and gait abnormalities can lead to it too. This includes, but is not limited to, flat feet, overpronation, bunions, and hammertoes. All of these conditions put extra stress on your bursa to the point of irritation, which results in bursitis.
Diagnosing
Physical exams are the standard for diagnosing foot bursitis. Your doctor will want to get an idea of the type of movements and activities your foot goes through on a given day. Things like the exercises you do, equipment you wear, and amount of standing or walking you do for your job all can have an impact.
For situations that involve traumatic injuries, the doctor may order tests to rule out any fractures or other injuries. Depending on the extent of everything going on, you may be referred to a specialist. Either way, getting an early diagnosis can save you from a ton of pain in the future.
Treatment
Almost everyone who has foot bursitis can get better with just conservative treatment. You may want to rest your foot in the beginning, especially when your symptoms set in. But you’ll want to do more than that if you really want to take care of the bursitis.
Stretching is an excellent way to heal your heel and relieve the pain, but knowing which stretches you should do is key. Most doctors will recommend starting physical therapy for this exact reason. The physical therapist will guide you through the most effective stretches and exercises, and tell you which ones are too risky.
PT’s are experts in movement, which means they know to focus on more than just the heel, but your foot as a whole (and even a bit of the lower leg too.) Everything is connected and works together, so it doesn’t make sense to only target one area hoping for it to be beneficial. Plus, foot injuries are known to make people start walking differently. Whether that’s a conscious choice or not, it’ll have a ripple effect and create a whole bunch of other problems down the line. Your therapist will work with you on your gait and balance so you can avoid that situation altogether.
Gout
Gout is one of those health conditions that you hear about on TV commercials but isn’t really talked about much until you experience it yourself. Similar to osteoarthritis, gout is a type of inflammatory arthritis. It causes pain and swelling in your joints, typically the one in your big toe, but it can affect the others too. Instead of being caused by wear and tear, though, it happens because there’s a buildup of uric acid in your foot.
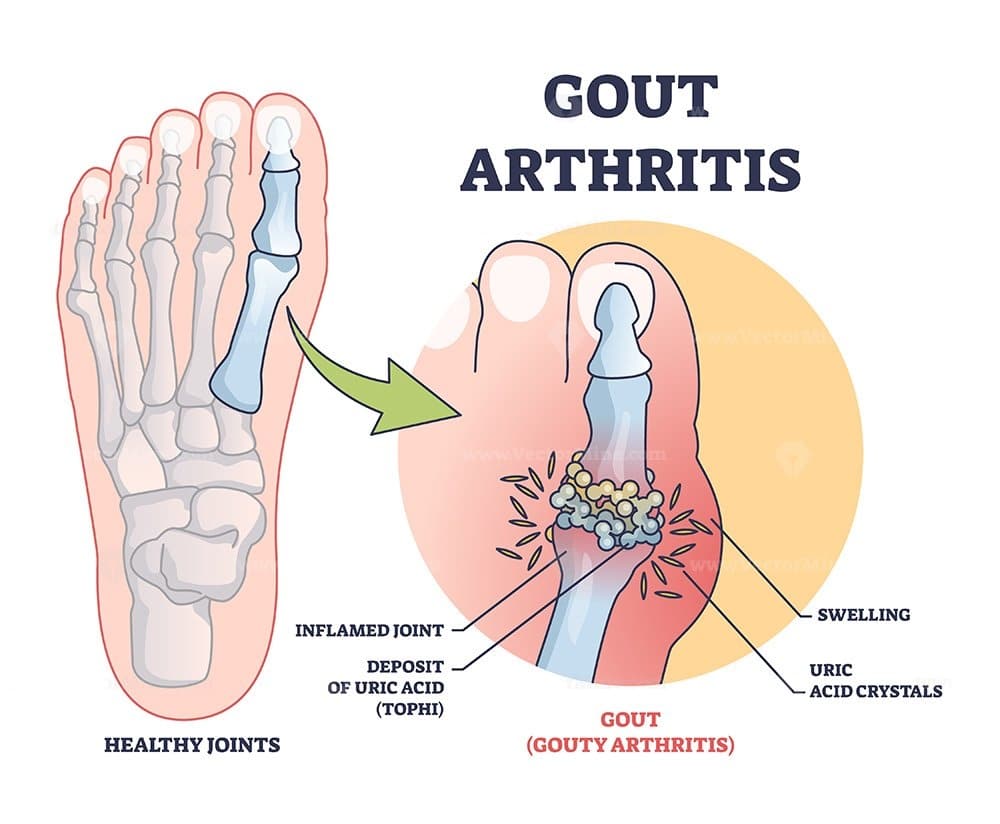
Your body naturally makes uric acid on its own when it breaks down chemicals (called purines) in certain foods and drinks. Usually, your kidneys filter it out of your system, but sometimes it can’t get filtered out or your body makes too much. The uric acid crystals end up settling into your joints and clump together. That’s when you start getting episodes of pain, swelling, and a bunch of other fun symptoms.
Symptoms
The thing about gout is the symptoms come and go in episodes (referred to as gout attacks or flares.) They’re extremely painful and can come on quite suddenly, often overnight.
During these attacks, you may notice a range of different symptoms. The most prominent and typically consistent one is an intense pain in your toe joint. Your skin will likely feel warm or like your joint is on fire. There’s usually some redness or discoloration that comes along with it as well.
When those sharp uric acid crystals build up, it can cause a lot of swelling inside your joint. And yes, you read that right. The crystals are sharp, so even with a light touch, it’ll feel pretty tender. They can also make your joints stiff, which of course can make it difficult for you to walk.
Generally, gout flares last around a week or two. Some might last more than others, and some might be more mild compared to the previous ones. You may not even experience any symptoms between attacks.
Causes
Gout can happen to anyone, but men get it 3x more than women (who usually don’t develop it until after they’ve gone into menopause.) Certain health conditions also put you at a greater risk, like obesity, diabetes, or congestive heart failure. Genetics can also play a part. You’re more likely to get gout if your biological parents or grandparents had it.
If you temporarily have high uric acid levels, it doesn’t necessarily mean you’re going to get gout. But if you eat or drink foods that are high in purines on a regular basis, it can become hard for your body to handle all of that uric acid. Sweets, sugary drinks, and anything with high fructose corn syrup are big triggers for gout. The same goes for alcohol and game meats as well.
Diagnosing
You can get your gout diagnosed with a simple visit to your doctor. They’ll want to take a look at your foot for the obvious signs, but their diagnosis will come from equal parts physical findings as well information they gather. Make sure to tell them when you first noticed any symptoms and how often the flare ups come and go.
They’ll also want to know more about your diet. Meals consisting largely of red meat (and even certain seafood) or a lot of sweets are big indicators of gout. Imaging usually isn’t necessary, unless the doctor is concerned about changes to your joint. If they’re still a bit unsure, they can do a blood test or aspirate your joint to check your uric acid levels.
Treatment
While there isn’t a cure for gout, it is treatable. Treatment usually involves a combination of things, especially during those flare ups. Some people might get more frequent or more severe attacks as their body adjusts to everything. If left untreated, you could develop severe arthritis which can actually change the shape of your joints. That’s why it’s best to take a proactive approach.
The first thing you’ll want to do is try to lower the purines in your diet. Consuming fewer foods and drinks with a high purine content will help reduce the crystals from building up in your foot. You might even eat some new foods that actually lowers your uric acid levels.
It’s also a good idea to start physical therapy. PT can help you manage the symptoms of your gout and even prevent future flare ups. The therapist will create a treatment plan that focuses on maintaining the flexibility and range of motion of your joint and foot as a whole. They’ll teach you strengthening exercises and work on improving your balance as well.
Dislocated Toes
When you think about all the body parts you can dislocate, your toes probably aren’t high on the list. Nevertheless, dislocated toes are actually quite common, especially for older adults and athletes. Toe dislocations happen when the bones of your toe are forced out of their regular position.
Dislocations are considered a complete separation of the bones in your toe joint. The ligaments that normally hold your bones together often get torn in the process. Toes dislocations are so common because they can be caused by something simple like jamming your toe or from an injury that forces your toe to bend or twist.
Symptoms
Even though your toes are tiny compared to your arm or knee, they’re still painful when they become dislocated. You may actually be surprised by how sharp the pain feels. There’s usually swelling, some bruising, and evening an audible tearing noise that can happen as well. Don’t freak out if your toe looks crooked, that’s completely normal with a dislocation.
As you may remember, each of your toes has 3 bones (called phalanges), except your big toe, which has 2 big phalanges. Dislocations can happen at the joints when your phalanges come together. These joints are called the distal interphalangeal (outer joint), proximal interphalangeal (middle joint), and metatarsophalangeal (where the toe meets your foot).
When your toe is forced out of its normal alignment, it can’t move like it should. Because of this, walking and moving, or just putting weight on your foot, becomes very difficult. Depending on how the dislocation happened, you could even have a fracture or chip in one of your bones. You might start to notice some numbness or a tingling pins and needles like sensation in your toe as well.
Causes
Anyone can dislocate any one of their toes, but more often than not it’s the second “pointer” toe that is the victim. A lot of children and athletes dislocate their toes because their activities are on the stressful, riskier side. It’s far too easy for them to accidentally bend and twist a toe or jam them somehow.
Adults over the age of 65 also have a higher risk of toe dislocations, usually from being unsteady or uncoordinated. Certain health conditions, like rheumatoid arthritis or hammer toe, can cause your joints to contract to the point that they eventually become dislocated. Activities that involve repetitive movements can wear down your joints as well, making it easier for dislocations to occur.
Diagnosing
The tricky thing about dislocating your toe is the symptoms are so similar to a sprained, fractured, or broken toe, so it’s important to see your doctor right away. They’ll start by gently manipulating your toe and feeling for any signs of a dislocation or possible break. If your joint feels unstable, it’s generally a sign that it’s dislocated.
After they examine your foot, the doctor will want to do an X-ray to confirm everything. This will also help make sure there isn’t a fracture or break in the bone either. In rare cases, your dislocation can pinch a blood vessel, which could permanently damage your toe. So, it’s imperative that your doctor makes a proper (and thorough) diagnosis.
Treatment
The first thing that you should do when you dislocate your toe is see a doctor. Do not, under any circumstance, try to put your toe back in place yourself. There’s plenty of nerves and veins running through there that you don’t want to risk any complications. Your doctor will do something called a reduction to realign your bones safely.
After your toe is back in place, your real treatment plan can begin. If you choose to start physical therapy, you can focus on restoring the mobility in your foot. This is important to do early on, especially before your walking starts to change. You’ll learn exercises to build up your strength and work to improve your balance.
Most people take anywhere from 6 to 12 weeks to fully recover, depending on the severity of their injury and how quickly they started (and adhered to) physical therapy. Once you dislocate your toe, it can easily happen again, so don’t rush the healing process. Under your therapist’s guidance, you’ll slowly start to return to your normal activities.
Click here to learn more about how Borja Physical Therapy can help treat your foot injury.