Believe it or not, hip injuries aren’t just for elderly folks. That’s right- they can happen to anyone. As one of the largest joints in your body, your hips are constantly being used to move, balance, and support your weight. Such an important structure with a ton of responsibilities, it’s no wonder so many people have hip injuries. This article will attempt to discuss the most common hip injuries and what you can do about them.
Basic Anatomy
First, let’s go over some basic anatomy. There are 2 bones that form your hip: the thigh bone or femur and the hip bone or pelvis. They come together to form a ball and socket type joint on each side of your hip called the acetabulofemoral joint.

Surrounding both joints are some large muscles that support your hip and help you move. The muscles in question include your gluteals, iliopsoas, hamstrings, quadriceps, and adductor muscles.
Next is your tendons, which are bands of tissue that connect your muscles to your bones. As for ligaments, they connect bones to other bones and give your body structure. Your tendons and ligaments both support your hip joint and help keep everything stable.
Then there’s cartilage, which is on the ends of each of your bones. In regards to the hip, you have a smooth, thin layer on top of your thigh bone and covering the inside of the pelvis socket. Cartilage acts as a shock absorber whenever you move and walk around. There’s also a fluid filled sac called a bursa that cushions all of your muscles, tendons, and bones in your joints as well.
Now that you’ve had a brief overview on the different parts of your hip, let’s take a closer look at some muscle injuries.
Muscle Injuries
Your muscles are kind of a big deal- and not just in a ‘let’s flex to show off those legs’ kind of a way. They do a lot of heavy lifting (literally and figuratively) to keep you moving. They’re like your body’s own support staff, providing you with strength and stability when you need it the most. All in all, there are 5 main team members, or in this case, groups of hip muscles, each with different responsibilities. They include your hip flexors, extensors, abductors, adductors, and rotators. Some help you walk or sit down, while others assist you in getting out of certain positions.
In order for you to function, your muscles have to work closely with your tendons. Think of them as personal assistants. They connect your muscles to the bones around your hip, pelvis, lower back, and thigh. If they get weak and can’t pull their own weight (once again, literally and figuratively), then your hip isn’t being supported properly and that’s when you get injured.
Hip Adductor Strain
One of the most common types of hip injuries is a strain, especially involving your adductors. You probably know this more as a groin strain or pulled groin. Basically, a hip adductor strain happens when one of your inner thigh muscles or tendons gets stretched out too far, is overused, or ends up tearing. It’s similar to a hip flexor strain, which you’ll read more about in a bit. But first, let’s continue…

There’s 5 different adductor muscles: adductor brevis, adductor longus, pectineus, adductor magnus, and gracilis. The first 3 are short muscles, while the last 2 are longer. Most of the time, it’s your adductor longus muscle (the one that attaches just above your knee) that gets strained.
Hip adductors are in charge of adduction, which is just a fancy way to describe moving your stretched out leg back to the center of your body. They also keep your hip and pelvis stabilized whenever you try to walk or run. Strains usually happen when you have poor flexibility or make quick sudden movements, like randomly deciding to sprint or kick something.
Symptoms
One of the biggest signs that you’ve strained your hip adductor is if you get a sharp pain in your groin out of nowhere. Normally, it tends to get worse when you move your hip or bring your legs together. You might even get pain down the inside of your thigh. You’ll likely see some pretty obvious swelling and bruising after about a day or two, especially around the strained muscle itself.
Muscle strains are graded on a scale from 1 to 3, depending on how much the muscle has stretched and if there’s a tear.
- Grade 1. Grade 1 strains are considered pretty mild. You’ll have some pain with just a slight loss in your strength and movement. They’ll often be described as a “pulled muscle”.
- Grade 2. You’ve upgraded to a grade 2 strain when there’s moderate damage to your muscle fibers. You’ll also have some overall weakness in your hip, along with the pain and tenderness.
- Grade 3. If you have a grade 3 strain, then there’s a severe or complete tear in your adductor muscle. You’ll be in a lot of pain and won’t be able to move very well either.
Stretching and tearing can happen anywhere along the muscle. Tears in the middle of your muscle are usually fairly straightforward, but can get more problematic the closer they are to your tendon. Those kinds of strains take longer to heal and can become chronic if you’re not careful. They may even cause some secondary issues too.
Causes
Adductor strains are simply a result of too much stress on your hip. When the muscles contract too quickly or too forcefully, they can overstretch and even tear. Typically, repetitive and excessive movements are to blame. The same can be said for activities that have a lot of twisting, turning, or direction changes. A direct blow to the groin can also do the job as well.
For the most part, groin strains happen randomly. There are a few risk factors that can increase your likelihood though. This includes things like not warming up properly before physical activities or having poor posture.
Diagnosing
A doctor can diagnose hip adductor strains by doing an exam. They’ll ask how you got the injury, if your symptoms have progressed, and what makes your pain worse. Then they’ll perform several tests, like checking your strength and range of motion.
A more hands-on thing the doctor will do is press on and around your hip to see if there’s pain anywhere besides your adductor muscles. They’ll also have you do certain movements, like squatting and jumping. This gives them an opportunity to observe your mobility and posture, and see if there’s anything restricting your motion.
Unfortunately, a physical exam only does so much. It doesn’t show how severe the strain is, or what kind of swelling or tissue damage there might be. In these situations, your doctor will order imaging to get a better idea of what’s going on.
Treatment
Dealing with a hip adductor strain can be tricky, but most people respond exceptionally well from early treatment with physical therapy.
At PT, you’ll learn to manage your symptoms while you let your injury heal. The therapist will help you modify any of your normal daily activities and tasks that might be risky in this stage of recovery. It’s crucial that you don’t push through any kind of pain with a groin strain or your short term injury will turn into a long term problem.
Once your pain and swelling has improved, it’s time to start toward your next goal. You’ll work with the therapist to regain your normal movement, flexibility, and muscle strength in your hip. As that movement comes back, you’ll get new exercises that build your strength, endurance, and balance. These exercises will also help your walking gait pattern too.
The last stage of your recovery will focus on returning to your favorite activities or workout routines. Your PT will guide you through all the steps in order to make that happen.
Hip Flexor Strain
Now that you know about hip adductor strains, let’s move on to hip flexor strains.
When you have a hip flexor strain, it’s referring to a group of muscles that run across the bottom of your abdomen and down the tops of your thighs. These 5 muscles are called the iliacus, psoas, pectineus, rectus remoris, and sartorius muscles. They’re the muscles that let you lift your knee and bend your hip. If you overuse one of them, they can stretch beyond their limit and tear apart.

Think of a hip flexor strain like you’re trying to tie down some luggage with a bungee cord. A brand spankin’ new bungee cord has plenty of give and stretch (just like healthy muscles) and is ready to keep all of your belongings secure. Now think about your old, tired, beat up bungee cords. You know, the ones that you’re honestly surprised even made it this far in one piece. Using them too much or yanking on them too hard can cause the elastic fibers to pull apart, just like your muscles. So, a strain happens when thousands of these bungee cords (muscles) are overstretched and then tear.
Symptoms
After straining your hip flexor, you’ll likely notice a sharp pain in the front of your hip and possibly into your groin. It’ll also be nearly impossible to move or even walk without having pain to some degree. Don’t be surprised if your hip starts to feel weak or unstable either. That’s another common symptom.
Hip flexor strains are graded very similarly to hip adductor strains.
- Grade 1. Grade 1 strains are the most mild of the three. Your muscles have only overstretched enough to cause minor tears and damage to a few fibers.
- Grade 2. Grade 2 strains are a bit more serious. The damage from the stretching and tearing can potentially affect your hip flexors’ ability to function.
- Grade 3. Lastly are grade 3 strains, which are the most severe. Your muscle fibers are completely torn and you aren’t able to walk without limping.
Most hip flexor strains are a grade 2. Typically, the grade of your strain matches up with the intensity of your symptoms. That means things like having trouble walking, pulling in your hip, or even muscle spasms can be more dramatic with grade 3 strains compared to grade 1 strains.
Causes
Anyone can strain their hip flexors, but it’s more common if you’re active. You don’t have to play sports or hit the gym all the time to strain them though, it can happen by simply overexerting yourself all of a sudden.
A big thing that can strain your hip flexors is overuse. Like a lot of injuries, repeating the same motion over and over again puts a ton of stress on your muscles. Whether it’s happening at work or during hobbies at home, after a while, your muscle fibers can’t take the strain anymore and end up tearing.
Traumatic events, like a fall or a car accident can also cause a hip flexor strain. This is especially true if you tense up or brace yourself before impact.
Diagnosing
Luckily, all you need to do for a hip flexor strain is schedule an exam with your doctor.
Since a lot of these strains usually come from physical activity, it’s important to pin down what exactly caused your injury. That’s why you should make sure to tell your doctor what you were doing and when you first noticed any symptoms.
Depending on the severity of the strain, you may need some imaging tests to confirm your diagnosis and rule out other injuries. An ultrasound can be used to check for tears or if there’s any fluid buildup around your muscle, . MRI’s on the other hand will let you know if there’s damage to your tendons or ligaments.
Treatment
The best way to treat hip flexor strains is with physical therapy. If you don’t do anything at all, you can end up causing an early onset of osteoarthritis in your hip, which is a whole other issue. So, it’s a good idea not to wait on starting PT.
At physical therapy, you’ll work on strengthening your hip flexor muscles and maintaining your flexibility (even if that’s not a lot at the moment.) Your therapist will help you through your entire plan of care so you can return back to your normal activities or workouts safely, especially anything that stresses your legs and hips. You should see progress within a week or two, depending on how bad your strain is.
In order to avoid another strain, you’ll want to stretch and warm up before exercising or doing anything too physical. Being flexible means your muscles can stretch more without tearing, so you’ll be less likely to get injured. Just think of it as breaking in your favorite pair of jeans. You have to wear them a few times before they stretch a bit and feel comfortable. Your muscles are the same way. The more you “wear them” or in this case, gradually stretch them, the more give and flexibility you have when you move.
Hip Tendinitis
Muscle strains aren’t the only type of injury your hip can go through. Hip tendinitis, for one, is very common. It’s a condition characterized by inflammation in at least one of the tendons in your hips. These tendons connect muscles to bones, like your gluteals and adductors to your pelvis and thigh bone. When those muscles get overworked, your tendons become inflamed, which is what ends up becoming tendinitis.

Symptoms
Possibly the biggest sign that you’re dealing with tendinitis is if your hip gradually starts to become tender and painful, especially at the spot where your tendon attaches to your hip bone. If you let things go untreated, your pain will get way worse and could even start to affect your ability to move. Essentially what will end up happening is your tissue will get more stressed and continue breaking down, turning tiny tears in your tendons even bigger.
Some other things you might notice is stiffness, particularly in the morning, and possibly a snapping or clicking sound when you walk. And since your joint is getting weaker, you’re also more likely to experience other hip injuries down the line.
Causes
Anyone can get hip tendinitis, but it’s more common if you’re an adult because your body naturally gets worn over time. This is called degeneration, which is when your tendons break down and become weaker as you age.
Flare ups will happen a lot, especially when you really stress your tendon by doing the same motion over and over again. Normal everyday activities, like going up and down the stairs or even walking, can cause hip tendinitis and will quickly become very painful to do. These kinds of movements put stress on your tendons, especially if you don’t stretch properly beforehand.
Diagnosing
With tendinitis, your doctor will examine your hip for signs of pain or discomfort. They may also order some imaging tests like an MRI, X-ray, or bone scan to confirm the cause and rule out any other issues.
Treatment
When it comes to hip tendinitis, you won’t ever be able to fully heal if you’re still aggravating the tendon. You have to give it a chance to calm down and recover, which means stopping whatever activities are causing the tendinitis in the first place. Don’t worry, it’s not permanent, just until your pain and inflammation subsides.
Starting physical therapy soon after your injury is a great idea so you can stretch out and strengthen your hip while it heals. Stretching promotes blood flow to any injured muscles and tendons you may have. This helps speed up your recovery time and decreases your chances of injuring another tendon or muscle. At PT, you’ll learn these kinds of stretches and get a customized exercise program as well.
One of the most important things your therapist will do is help you change up any of the activities you do on a daily basis that might be risky or dangerous. That way, you can still do the things you need to do at home or work without making your tendinitis worse. The PT will also teach you how to use exercise equipment so your muscles and tendons have time to gradually build up without tearing in the process.
Hip Impingement
The next injury we’ll take a look at is hip impingement. Hip impingement, or its fancy medical name, femoroacetabular impingement (FAI), is a condition where the bones that are part of that “ball and socket joint” rub and pinch together.

Normally, the round head of your thigh bone fits comfortably into the socket of your pelvis without any issue, thus forming your hip joint. But when you have impingement, those two bones grind against each other instead of gliding smoothly. If you don’t do anything about it, you can end up permanently damaging your hip joint.
Symptoms
As you can imagine, any time bones rub together, it’s pretty excruciating. Hip impingement is no exception. The pain can make even simple things like walking or moving almost unbearable.
After a while, all that rubbing will start to wear down the cartilage in your joint. Cartilage acts as a cushion between two bones. So, the longer you live with hip impingement, the more your cartilage gets damaged, which usually means your symptoms will get worse too.
Typically with impingement, you feel a constant dull ache around the side of your hip. It can also radiate toward your thigh, groin, or butt. People usually describe the pain similar to pressing on a deep tender bruise.
You’ll probably notice that your pain gets worse during physical activities, especially if you’re stressing your hips a lot with things like jumping, lunging, or squatting. Laying on your side can also make your pain worse. The same goes for sitting too long. All of these can turn your normally aching pain into a sharp, stabbing feeling.
If you let your hip impingement go on long enough, it won’t just be the pain you’ll have to worry about. You’ll start to notice it becoming more difficult to move or use your hip. You could even tear the rim of cartilage that lines your hip socket (called the labrum.) And if that wasn’t enough, you’re also more likely to develop osteoarthritis from all that cartilage being worn down.
Causes
Hip impingement happens when your two hip bones catch and rub together. Usually, it’s because there’s a bone spur, which can be something that you’re simply born with or they can develop naturally over time.
There are 3 different types of hip impingement. The first type, called cam impingement, happens when there’s extra bone growth on the top of your femur. Next is pincer impingement, which also involves an extra bony growth, but this time it’s in your hip socket. Lastly, there’s combined impingement, which is a combo between the first 2 types.
Impingement can happen to anyone, but males usually get cam impingement and females get pincer or combined. Athletes also have a higher risk of developing hip impingement, especially if their sport puts a large amount of pressure on their hips.
Diagnosing
The best way to diagnose hip impingement is with an exam and some imaging tests. Imaging, like an x-ray or MRI, will show if there’s any issues inside and around your hip joint. The doctor might also try injecting your hip with a small amount of local anesthetic. If numbing the joint relieves your pain or stiffness, then it’s likely that you have impingement.
There’s a physical test your doctor can do too. Essentially, they’ll move your hip into a series of positions that puts pressure on different parts of your hip. If you feel pain at any point while they’re moving you, then that’s a clear indication of impingement.
Treatment
The most important part of treating hip impingement is preventing more damage to your hip while managing your symptoms at the same time. That’s why physical therapy is such a great course of action.
During physical therapy, you’ll focus on strengthening the muscles around your hip. Getting all of those muscles stronger means more stability. More stability means more protection for your hip. Plus, you’ll be able to start moving better too.
A key part of physical therapy that you might not know about is activity modification. Basically what that means is learning how to change how you do certain movements or activities that might be risky for your hip. Your PT may even have you avoid some of the more dangerous ones altogether.
You might not necessarily be able to stop hip impingement, but you can help prevent the pain from getting worse. Treating your impingement sooner rather than later is also the best way to avoid any complications from happening, like a labral tear.
Snapping Hip Syndrome
Another common tendon injury is snapping hip syndrome. This is a condition where one of your tendons gets tight and swollen, which causes your hip to move abnormally. It gets the name snapping hip because as your tendon tightens, it starts to ‘snap’ over your hip joint whenever you walk or get up from a chair. A lot of times you can actually hear an audible snapping or popping sound if you listen for it.
Outside Of The Hip
Generally, you’re more likely to experience snapping on the outside of your hip, specifically where your iliotibial (IT) band passes over the femur.

Take a look at the illustration above. When your hip is straight, your IT band sits behind the femur (as shown in the first picture.) But when you bend your hip, it moves over the femur and sits in front of it. Your IT band is like a stretched out rubber band, it’s always tight, and the head of your femur naturally sticks out a bit. So, when your IT band moves back and forth across, it makes a snapping sound.
Front Of The Hip
There’s two other tendons that are typically affected by snapping hip syndrome, one being your rectus femoris tendon. This tendon runs from the front of your thigh all the way to your pelvis. It shifts across the head of your thigh bone when you bend your hip, then back to the side when you straighten again. All of the back and forth over the thigh bone is what’s causing the ‘snap.’
The other tendon is the iliopsoas. This tendon is actually made up of 2 muscles, psoas and iliacus, that merge together to form a tendon. It attaches to your femur and runs along the front of your hip to deep within your pelvis. Whenever you move, it catches on the bony parts sticking out from the front of your pelvis, causing (you guessed it) a snapping sound.
Symptoms
Two of the biggest complaints that usually come with snapping hip syndrome is pain and difficulty walking. They’re often paired with muscle weakness and a deep soreness that can be felt in your groin.
And it doesn’t just stop at your hip either. It’s common to have pain and stiffness up into the lower part of your back. You’ll probably get some tightness when you’re doing activities that have a lot of flexing and extending too.
With enough time, snapping hip can even damage your cartilage. If it’s the iliopsoas tendon that’s involved, part of the snapping is happening over your labrum, which will eventually begin tearing because of all the rubbing. Before you know it, that deep pain in your groin will be way, way worse.
It’s likely that you’ll also start to notice some problems with keeping your posture. Oftentimes, this kind of issue leads to something called lordosis. Lordosis is a condition where the curve of your lumbar spine has changed and now curves excessively inward. Of course, this change means there’s more pressure on different parts of your spine, which typically leads to arthritis.
Speaking of arthritis, choosing to ignore snapping hip syndrome can actually end up causing hip bursitis. You’ll learn more later on in this article, but basically, bursitis is inflammation of your bursa, which is a sac filled with fluid inside your hip joint. It’s what normally allows your muscles to move smoothly over your bones, but with bursitis, it makes moving a lot more challenging (and painful!)
Causes
The cause of snapping hip syndrome can vary, but it’s usually from doing repetitive movements or simply overuse.
Athletes who heavily rely on their hip flexors, like dancers or gymnasts, are particularly prone to this injury. If you have to sit for long periods of time, either at work or for a hobby, you’re also at a higher risk. This applies to activities that have similar positioning too, like bicycling or doing sit ups.
One of the biggest contributing factors to snapping hip syndrome, though, is hip replacement surgery. So much so that it happens to more than 4% of all hip replacements, which might not seem like much, but in actuality is quite high compared to other post-op complications.
When you get a hip replacement, you have to do a lot of walking up and down stairs and practicing getting in and out of cars as part of your recovery. Movements like these typically trigger pain because your tendons are now rubbing over the metal shell of your new hip. Most people complain of pain near their groin and occasionally radiating down into their thigh.
Diagnosing
There are a few ways doctors can diagnose snapping hip syndrome. They’ll start with an exam, where they can discuss your symptoms and which activities seem to cause your tendon to snag. They’ll also see whether they can recreate the snapping by having you stand and move your hip in different directions. In some cases, the doctor can actually feel the tendon moving when you extend or bend your hip.
Imaging, like x-rays or MRI scans, aren’t very helpful in identifying snapping hip syndrome, but they can be used to rule out other issues with your joint.
Treatment
Treating snapping hip syndrome doesn’t necessarily mean you need anything invasive like a surgery or even steroid injections. Most of the time, you can heal through rest, activity modification, and a good strengthening program. Luckily, this is easily doable with physical therapy.
The first two of those things go fairly hand in hand. It’s important that you back off doing any repetitive or aggressive hip movements, basically anything that will aggravate your tendons, so they can rest and recover. Ideally, you’ll want to avoid these types of motions all together, but if they’re a requirement for your job or hobbies, then your therapist will help you find safer ways to do them.
The PT will also create a customized exercise program just for you and your situation. It’ll focus on stretching and strengthening the muscles surrounding your hip. As you master the exercises, you’ll start to notice some indirect effects regarding your symptoms. For one, your pain will become much more manageable. The swelling in your tendon will also go down as well. Soon enough, and with a little bit of practice, you’ll be able to return back to your normal activities.
Ligament Injuries
Now, it’s time to take a look at your ligaments. Ligaments are just strong pieces of fiber that connect two bones together. There are 5 main ligaments in your hip: iliofemoral, pubofemoral, ischiofemoral, ligamentum teres, and zona orbicularis. These ligaments connect your thigh bone to your pelvis. All of them, along with your joint capsule, stabilize and control how your hip moves, which includes preventing you from doing any movements that could damage or dislocate your hip.
IT Band Syndrome
As hip injuries go, one of the most common (and kind of unique) is IT band syndrome. Your IT band, or iliotibial band, is a band of tissue that runs from your hip all the way down to your knee. It gets mistaken as a tendon quite often because of how it functions, but it’s actually a ligament… and technically a muscle too. You get this kind of injury when your IT band becomes swollen and irritated from rubbing against your hip… or your knee. It can affect either side of your body, or both at the same time, depending. Like we said, ‘kind of unique.’

Now for the ‘common’ part. As many as 30% of all adults experience IT band syndrome at some point throughout their life. It’s actually one of the leading causes of hip pain and knee pain as well.
Interestingly enough, IT band syndrome is a very common diagnosis amongst US Marines. More than 20% develop it during training. Runners are also very prone to the injury as well, making up close to 12% of all running injuries.
Symptoms
A tight, irritated IT band can cause quite a few different symptoms, the most prevalent being hip pain. Because of where it’s attached, your IT band rubs against the top of your femur every time you move. All that friction causes your IT band to become irritated and inflamed, which is as painful as it sounds. You might also hear a snapping noise, similar to snapping hip syndrome. That snapping and clicking can happen closer down near the outside of your knee as well.
Speaking of your knees, it’s very likely that they’ll bother you too, especially on the outside near the bottom of your thigh bone. Just like with your hip, your IT band gets inflamed when it rubs against the lateral (outside) part of your knee. That’s why it hurts to bend and straighten your knee.
At first, you’ll probably notice the pain after you’re done exercising. As your condition gets worse though, you’ll feel it throughout the entire workout. Eventually, the pain will be there when you’re resting too. Most people describe their pain as an aching burning sensation, but turns noticeably sharper the more you exercise.
Causes
You know that IT band syndrome happens when your IT band gets swollen and irritated from being stretched too tight and rubbing against bone. But, why exactly does it tighten in the first place?
Usually, the reason is mechanical. An example of this would be if you had excessive foot pronation, meaning your feet naturally rotate outward. Even though this rotation is in your foot, it actually pulls on your IT band and causes it to stretch, which also brings it closer to your hip and knee bones.
Another culprit is weak hip abductors. Your abductors are the muscles responsible for turning your hip away from your body. If they’re weakened for any reason, you won’t be able to rotate fully, causing your IT band to get strained and tighten in the process.
You could also have a type of arthritis that causes your knees to bend out when your feet are together, essentially making you bow legged. This, you guessed it, pulls on your IT band, tightening it as a result. And of course, you could just be one of those people who are born with a tighter IT band.
There’s a few reasons your tight IT band might start rubbing against your hip or knee bone.
A lot of the time it comes down to not taking care of yourself before or after physical activity. Most people don’t stretch well enough prior to exercising. Your IT band needs to get warmed up a bit before jumping into anything rigorous. That goes for not doing a proper cool down after you exercise as well. Pushing yourself too hard and not giving your body enough time to rest can be just as bad.
Diagnosing
Doctors can determine whether or not you have IT band syndrome by doing a simple exam. You’ll want to tell them where you’re feeling pain and describe the type of pain too. That way, they’ll have a better idea of how far the syndrome has progressed.
There’s also a test they can do called the Noble and Ober test. First, they’ll start by feeling the outside of your knee, near the lateral epicondyle, to see if that spot causes any pain. Next, they’ll move your hip away from your body while supporting your knee. Depending, your hip may or may not move very far. Lastly, they’ll move your knee in different directions to see what angles trigger pain.
If your doctor’s still unsure about the diagnosis, they may order an MRI to rule out a possible meniscus or ligament tear. These kinds of tears tend to mimic IT band syndrome, so an MRI can help tell the difference between the two. You might also get sent for an ultrasound, which will show how your IT band moves when you flex and extend your hip.
Treatment
When it comes to treating IT band syndrome, it all depends on how severe it is. You definitely don’t want to leave it untreated, though, or your pain will likely get worse. The good news is, you can heal your IT band syndrome with none other than physical therapy.
There are a few different ways your therapist can help. Probably the most important thing they’ll do is teach you strengthening exercises and stretches. These exercises will help relieve your hip pain, plus if there’s any pain in your knee too. As your plan of care progresses, you’ll learn new exercises that will help you as you continue to heal. Your therapist will also show you the best stretches to do before and after physical activity so you don’t make your injury worse. They may even encourage you to invest in something like resistance bands that can help.
Another thing you’ll do at physical therapy is focus on posture training. How you move and hold your body through the day, while being active or otherwise, all can influence your IT band syndrome. You’ll work to improve your posture so you can maintain it well after you complete physical therapy.
Close to 90% of people improve their IT band syndrome in as little as 4 to 8 weeks. Some more mild cases have even improved within 2 to 6 weeks.
Labral Tear
When it comes to hip injuries, one thing that can cause some major issues is cartilage, more specifically your labrum. The labrum is just a ring of cartilage that lines the inside of your hip joint. It acts as a shock absorber that stabilizes your hip. It’s also the reason your bones are able to move smoothly. When your labrum goes through enough trauma, it can get damaged and eventually tear.

Symptoms
There’s a few things you’ll notice right away when you have a labral tear. For starters, your hip will be in a lot of pain, especially when you move or bend. You might also feel unsteady while standing and walking. You may even hear a popping or clicking noise whenever you move your hip.
While some smaller labral tears may not have any symptoms, it’s the hip pain that really characterizes the injury. Depending on how bad the tear is, your pain could feel anywhere from a dull, constant ache to more of a deep bone bruise. Most people describe getting a stabbing, sharp pain during anything physical or when they’re in certain positions, like lying on their side. You could also get pain that radiates down your leg or into your lower back and groin.
It’s important to pay close attention to how you move, walk, and hold your body, because the pain can sometimes make you change the way you do those things without even realizing it. Any unconscious change to your posture or gait can put pressure on your muscles and make your hip injury worse.
Causes
Basically anything that puts too much stress on your hip can damage your joint enough to where it actually tears the labrum. So, it’s probably no surprise then that hip impingement is one of the leading causes. Since the bones in your hip joint pinch and rub together, they end up putting extra pressure on your labrum. Over time, that added pressure builds up and the smallest amount of friction can create a tear.
Another big cause is osteoarthritis, which is that “wear and tear” type of arthritis. When you have OA, the cartilage in your hip joint wears down over time from normal everyday stress. Eventually, it gets so worn down that your labrum will start to tear.
Like most injuries, trauma can be a huge contributing factor in labral tears. Anything with a strong force, like a fall or car accident, can instantly cause damage to your hip. Unfortunately, most of the time this kind of damage involves tearing cartilage.
Diagnosing
Your doctor can diagnose a labral tear through a few tests and a physical exam. During the exam, they’ll take a look at your hip and ask about your symptoms. The main thing they’re trying to find out is what types of movements or activities make your pain worse, and if there’s any other symptoms you notice.
Then they’ll take a closer look at how your hip moves. You’ll bend, stand, walk. They’ll even move your hip around in different positions to see if any of them hurt.
If your diagnosis is still unclear, the doctor may need some imaging done as well. Testing such as x-rays and MRI’s give a bigger picture of your joint and the surrounding area. This is a great way to figure out what exactly is going on with your hip.
Treatment
Surgery is the only way to actually heal a torn labrum, but most people can still live their normal day to day by managing their symptoms in noninvasive ways. When your labrum tears, your hip suddenly becomes unstable, so the goal is then to re-stabilize it. The best way to do this is through physical therapy.
At PT, the therapist will create a personalized exercise program designed for your kind of injury. They’ll choose exercises that strengthen the muscles surrounding your hip joint, specifically the ones in charge of supporting your body. Some exercises may seem more like stretches, which is by design. Those work more toward increasing your flexibility than solely your strength.
In the beginning, you might also need to make some changes to the way you do certain tasks or activities. If something causes pain, stiffness, or any other symptoms in your hip, you’ll want to avoid it. Unfortunately, you might not be able to avoid everything, especially if it’s a requirement at work or part of your everyday living. Instead of risking your hip getting worse, you can work with your physical therapist to find safe ways to do these movements.
Hip Sprain
Another type of ligament injury you might experience is a hip sprain. Not to be confused with the closely named hip strain, which involves your hip muscles. A hip sprain is when the ligaments around your hip get stretched or torn.
Ligaments are tough fibers that support your joints. They need to be tough in order to keep your bones connected to one another. So, when one of them stretches beyond their limit for one reason or another, it’s pretty noticeable. You might not even be able to move your hip like you normally would if your sprain is severe enough.

Symptoms
Like most hip injuries, when you sprain your hip, you’ll notice pain radiating over the joint. Usually, it’ll get worse the more you use your hip. It’s not unusual to have swelling, bruising, and tenderness along the hip either.
Your muscles may also feel stiff or like they’re spasming. In these situations, it can actually cause you to lose some flexibility and strength in your hip. It might even make it difficult for you to walk too.
Not all of your symptoms will necessarily be limited to right at your hip though. You may get a sharp stabbing type of pain in the back of your leg, along with some tenderness in your calf. Both areas might start to bruise or swell as well.
Causes
Most sprains are the direct result of trauma to your hip. This can come in the form of something like a car accident or collision while playing contact sports. Falls and sudden direction changes are super common too.
If you’ve sprained your hip in the past, then you’re more likely to do it again at some point in the future. There’s also plenty of other factors, like overuse from repetitive movements. Overstretching the ligaments in your hip before working out can be an issue. The same is true for not stretching enough. You can even sprain your hip by doing too much activity too quickly.
Diagnosing
The good thing about a hip sprain is that it’s easily diagnosable by your doctor. They’ll start by asking when your symptoms began, which activities bring them on, and what seems to make them worse.
Your doctor will do some physical tests too. First, they’ll check your range of motion by slowly moving your hip around. Then, they’ll test your muscle strength to see how well your hip is able to support your body. Last but not least is the stability of your hip joint, which goes hand in hand with muscle strength.
Depending on their findings, the doctor may order some imaging like an x-ray or MRI. These tests help rule out other serious hip injuries, especially if they share symptoms consistent with a hip sprain.
Treatment
Treating a hip sprain is similar to treating a knee or shoulder sprain, which means doing the RICE method for the first 72 hours. Usually, that’s not enough though, especially for moderate and severe hip sprains. In most cases, your doctor will recommend physical therapy.
It’ll start off a bit slow in the beginning while your hip is still tender and swollen. The physical therapist will use techniques like massage and manual therapy to help with your pain and inflammation. They’ll also give you your own specialized exercise program. The beauty of these exercises is that you can do them in the clinic and at home on your own. That means you can work on your strength and flexibility even on the days you don’t have PT.
Hip sprains generally respond to treatment fairly quickly. It could take anywhere from a few weeks to a couple months to fully recover, depending on the severity of the sprain. It’s extremely important to avoid going back to your regular activities until your hip has completely healed. For that very reason, your PT will work with you on activity modification.
Risky Activities
If you start doing the thing that caused your sprain in the first place, or something your body just isn’t quite ready for yet, then you’ll likely make your injury worse. So, what your therapist will do is look at all of your tasks and activities for a normal day and evaluate them. This includes anything work and hobby related too.
When the PT sees anything that’s a bit risky, they’ll show you ways to change or modify doing them so you won’t hurt yourself even further. This could be something like using a stool to kneel down on or changing the way you reach to grab items off the floor. They’ll also advise you on the best ways to warm up before certain activities.
Bone Injuries
As mentioned in the beginning of this article, there are 2 bones that make up your hip joint: the thigh bone and hip bone. On the ends of them is a smooth layer of cartilage, which is the whole reason you’re able to move your hip.
Most injuries involving your bones or cartilage are usually due to some sort of trauma or overuse. And while anyone can get a hip injury, some conditions, like ones that affect your bone health or balance, increase your likelihood.
Hip Dislocations
You’ve probably heard of dislocating your hip, but what does that really mean? Basically, it’s when your thigh bone pops out of the socket in your hip bone. Remember, your hip joint is a ball and socket type joint.
Like most dislocations, it’s very important to get your hip back in place right away (and by a medical professional.) Until you do, you’ll be in a lot of pain and your leg will pretty much be useless.

In the medical world, there’s 2 different types of dislocations.
If the ball of your thigh bone only shifted partially out of the socket, then you have a partial dislocation, or subluxation. These can range from mild to severe, and are fairly common for anyone that’s had a hip replacement or has hip dysplasia.
Now, if your thigh bone has completely shifted out of the socket, then you have a total dislocation, or luxation. By far, they’re the more complicated of the two types. They’re also incredibly painful and extremely debilitating.
Symptoms
From the outside, it may appear like your dislocated leg is locked in place, either turned outward or inward. About 90% of hip dislocations involve the hip being forced backward, leaving your foot and knee pointed inward. The rest are dislocations where your hip is forced forward out of the socket, with your foot and knee pointing outward.
Usually, it’s pretty obvious when your hips are out of alignment. One of your legs might look shorter, depending on the direction your hip is positioned. There might also be some discoloration or bruising too.
Along with your leg being popped out of place, you can expect a great deal of pain and swelling. Of course, you won’t be able to move your leg very well, if at all, and you certainly won’t be able to put any weight on it either. Some people even lose feeling in their hip and foot.
Secondary Injuries
In some cases, ligaments and nerves around your hip can be damaged during the dislocation. One nerve in particular is usually involved and that’s the sciatic nerve. Your sciatic nerve runs from your lower back all the way through your hip and down into your leg.
When you dislocate your hip, your bones shift from their normal spot. They can end up pressing against the nerve, causing something called sciatica. Sciatica is a common condition characterized by pain in the low back, hip and down through the leg.
If your femoral artery (which runs in front of your hip joint) gets damaged during the dislocation, then it can affect the blood supply to your bones. When this happens, you run the risk of developing osteonecrosis, which is where your bone tissue slowly dies because of the lack of blood flow. Once you get to this point, tiny fractures will start to form and eventually destroy the integrity of the bone.
It’s not uncommon to develop arthritis either. Arthritis is simply joint swelling and happens when your cartilage gets damaged, like from a hip dislocation. It’ll also increase your odds of needing a hip replacement at some point down the road too.
Causes
It takes a lot of force to push your joint out of its socket, so it’s not surprising that most hip dislocations are caused by some sort of trauma. Usually, this comes in the form of a car accident or a big fall. Sports and workplace injuries can also be to blame as well.
Occasionally, hip dislocations can be attributed to something called hip dysplasia. Hip dysplasia is a developmental condition where your thigh bone just doesn’t sit very well in your socket. Essentially, your hip sockets are more shallow compared to normal hips, making it easier to dislocate during ordinary activities or tasks. The ligaments and muscles around your hip won’t be as tight either, which means it’ll take less force to separate your bones.
Diagnosing
Hip dislocations are usually pretty obvious from a visual standpoint, so your doctor shouldn’t have a problem identifying yours. They’ll definitely want to do an exam too though, to make sure there isn’t any other damage or injuries. Depending on what they find, they may order imaging to get a better look at the positioning of your bones and the surrounding area.
Treatment
The most important thing to do after you’ve dislocated your hip is stop moving it. Not only is it extremely painful, but more than that, it can cause some pretty big complications the longer it’s left untreated. If you’ve dislocated your hip in the past, then it’ll likely happen again. Every time it gets dislocated, the muscles and ligaments that stabilize your hip joint get weaker. The cartilage lining your socket starts to erode too.
Speaking of cartilage, over 50% of people that have dislocated their hip end up developing arthritis. When you get arthritis in your hip, it often leads to needing a hip replacement at some point down the line. In turn, hip replacements are more likely to become dislocated. It’s a vicious circle.
After a hip dislocation, your doctor will do a maneuver called a reduction. In a nutshell, they’ll move your body in a few different directions to get your joint back into the right place. Since it takes a ton of force to dislocate your hip, it only makes sense that it takes a ton of force to move it back. While the reduction is a huge first step, it can still take a few months for your hip to fully heal.
The best way to deal with a dislocated hip is with physical therapy. They’ll teach you strengthening exercises that are safe to do, especially right after a hip reduction. In the beginning, you might be limited with what you should do movement wise, but as you heal, those restrictions will start to lessen.
Hip Fracture
One of the most serious bone injuries that you can go through is a hip fracture. When you fracture your hip, it means there’s a break in the upper part of your thigh bone (femur), close to where it meets your pelvis.
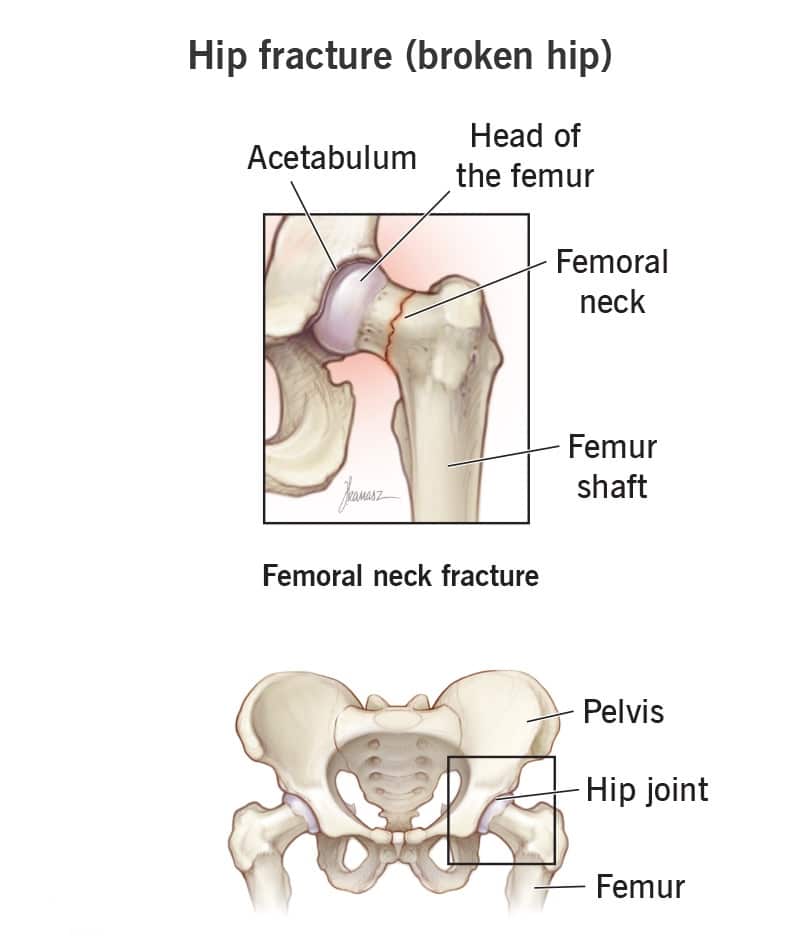
Your thigh bone, also known as the femur, is the longest and strongest bone in your body. Because it’s so darn strong, it takes a tremendous force to create a break. Most of the time, 98% to be exact, this kind of force comes in the form of a fall, especially in seniors who tend to have weaker bones. They can also be the result of high impact trauma, like a car accident or with long distance running.
Symptoms
Luckily, not every fall or high impact injury ends with a hip fracture. If you do happen to experience one though, there are some signs you should look out for.
One of the most obvious is pain. A lot of pain, actually. Any bone fracture is, at the very least, uncomfortable, but a break in your femur can be downright excruciating. You also won’t be able to put any weight on your injured leg either.
While these next 2 symptoms are kind of broad and can describe a lot of injuries, they can still indicate that you’ve got a hip fracture as long as they’re coupled with some more serious symptoms. The first is bruising on your thigh and the other is swelling near your hip.
With hip fractures in particular, your healthy leg may actually look longer than your injured leg. The injured one can also turn out and away from your body too.
If the break is near the top of your femur, then you run the risk of also breaking your pelvis, especially if you have osteoporosis. If the break is lower, then you can easily damage your knee, especially if you’ve had a knee replacement in the past.
Causes
Most people fracture their hip after some kind of traumatic event, like a fall or car accident. Adults that are 65 and older can even break their femur simply by falling just while they’re standing.
There are 5 different types of bone fractures you can get.
- Spiral Fracture. Like their name suggests, spiral fractures are characterized by a break that’s literally “spiraling” around your thigh bone.
- Transverse Fracture. A transverse fracture is when the break goes horizontally across your femur in a straight line.
- Oblique Fracture. When you have an oblique fracture, the break is at an angle across your femur.
- Comminuted Fracture. If your bone is broken up into 3 or more pieces, then you have a comminuted fracture.
- Compound Fracture. Compound fractures, also known as open fractures, are when the broken pieces of your bone break through the skin.
Luckily, it’s pretty tough to fracture your thigh bone since it’s so strong. If you have a health condition that makes your bones weaker, like osteoporosis, then there only needs to be a small force to break your hip. Stress injuries, like the kind long distance runners get, can also cause a fracture.
Diagnosing
The first thing your doctor will do to diagnose your hip fracture is carefully examine your hip and leg, then do some imaging. The most important test is going to be an x-ray of your hip so they can locate the break. You might also need an MRI to see if any of your nearby tissue got damaged, but that’s usually only needed for more severe injuries.
Treatment
Depending on which type of fracture you have, it can take several months to get back to normal.
Your hip will naturally go through different stages of healing. During the first 10 days, new bone and cartilage will start to develop and blood vessels will form. From that point on, all the newer bone is already remaking itself to become normal bone.
You’ll want to start physical therapy right after your injury to make the entire recovery process as smooth as possible.
Your Physical Therapy Journey
In the beginning, you’ll probably want some help at home for a week or two. You’ll focus on keeping your leg elevated to avoid swelling and finding comfortable ways to sleep. Then, you’ll start to work on moving throughout your house. This is where the physical therapist really comes into play.
Putting weight on your leg will be your first hurdle. More than likely, you’ll have to use crutches, a cane, or a walker to get around while you’re non-weight bearing. Your therapist will help you use them properly (and safely).
Once you’re up and moving, your biggest concern becomes avoiding falling or reinjuring your hip. Your physical therapist will switch up some of the things that you do or how you do them, as well as tell you how to modify different parts of your house so you won’t get hurt.
As you’re recovering, you’ll learn stretches and exercises designed specifically for hip fractures. Everything the PT teaches you will be safe yet effective. The exercises might seem fairly easy in the beginning, especially since you’re just starting to navigate putting weight on your leg. But, you’ll get new, more challenging exercises as you continue progressing.
You’ll also work with your therapist to meet various functional goals, like going up and down stairs and walking without any assistance. As your break heals and your thigh bone becomes stronger, the more stress it’ll be able to tolerate. Slowly but surely, you’ll work your way up to returning to doing all the normal activities you love.
Joint Osteoarthritis
Another joint condition you might experience that’s been mentioned a number of times throughout this article is arthritis, specifically osteoarthritis. Known as degenerative joint disease, osteoarthritis (OA for short) is the most common type of arthritis. OA develops when the cartilage that lines your hip joint gets so worn down that your bones start rubbing together, causing inflammation as a result.

Cartilage is a smooth, thin layer of protection that covers the ends of your bones. When you have osteoarthritis, the cartilage that normally protects your joints is wearing away. After a while, there’s nothing left to stop your bones from grinding against one another.
Symptoms
Osteoarthritis is a lot more common than people may think. More than 80% of adults actually have it, even if they don’t experience any symptoms.
There are 2 different types of osteoarthritis: primary and secondary. Primary OA is the direct result of wear and tear throughout your lifetime. Secondary OA develops indirectly after your joint gets damaged, whether that’s from a fall or another health condition.
The most common symptom when you have osteoarthritis, regardless of the type, is joint pain. You’ll likely notice it throughout the course of your day, especially while you’re on your feet. Your hip might be a little stiffer and restricted when you’re moving too because the cartilage is so worn down.
You might get some swelling outside of the joint itself that tends to come and go for no apparent reason. The look of your hip can seem noticeably different as well or even slightly deformed. A lot of people also say their hip doesn’t feel as strong or stable as it normally should.
Causes
Unfortunately, no one knows the exact cause of hip OA. Medical experts have an idea of some things that contribute to why it develops though.
With primary osteoarthritis, degeneration happens slowly over time. So, your joints naturally go through more wear and tear as you age, which accelerates how fast the cartilage in your hip breaks down.
As for secondary OA, trauma is usually to blame. Basically, anything that involves directly damaging your hip joint can lead to osteoarthritis down the line. This includes, but isn’t limited to, falls, car accidents, and collisions during contact sports.
While anyone can develop osteoarthritis, it’s much more common for postmenopausal women and adults over the age of 50. There also seems to be a link between OA and other kinds of arthritis, especially the inflammatory ones like rheumatoid or psoriatic arthritis.
Being overweight is especially risky for your hips since they hold the majority of your weight. Extra body weight means extra stress on your joints, which speeds up how quickly your cartilage breaks down. So, any type of weight bearing activities that you do, like running, walking, or even just standing upright, puts close to 4 times the force of your body weight onto your hips. It’s even more if you’re doing anything that involves jumping.
Diagnosing
There are a few ways that doctors can tell if you have hip OA. First, they’ll do a physical exam to take a closer look at your hip. Make sure to tell them when you first noticed any symptoms, what types of activities make them worse, and if they come and go or stay fairly constant throughout the day.
The best way to definitively diagnose osteoarthritis though is with imaging tests. The beauty of getting x-rays done is they’ll show you just how close your bones are to each other. Plus, you’ll be able to see the condition of the cartilage in your hip joint. The more worn down it is, the more severe your OA is.
Treatment
The bad news is once you develop osteoarthritis, you can’t get rid of it. There is no magical cure and you can’t regrow worn down cartilage. But the good news is you have plenty of treatment options that will help you manage your symptoms long term. One of the most effective is with physical therapy.
Exercising is the #1 way to relieve stiffness caused by OA, but sometimes that’s easier said than done. In the beginning, it can be painful to move your hips. Plus, you might not even know where to start with your workouts. That’s where PT comes in.
Your therapist will make everything easy and straightforward. You’ll learn simple exercises, most of which focus on strengthening the muscles around your hip. The stronger you can make those muscles, the more they’ll be able to keep your hip stable and supported.
As you get further into your plan of care, you’ll learn new, more advanced exercises. This doesn’t mean they’ll be difficult, rather the old exercises will just seem way too easy and almost like they’re not doing anything anymore.
Getting Back To Normal
For the most part, your biggest goal (aside from having less pain) is going to be returning to your favorite activities. Your PT will help you work to reach that goal. Keep in mind, though, slow and steady wins the race.
Before you can jump into anything face-paced or rigorous, you’ll start with lower impact activities, like walking or biking. You’ll even be able to do weight training. For some people, that might seem intimidating, but your therapist will be there every step of the way. Don’t be surprised if they suggest wearing orthotics in your shoes. Inserts help support and stabilize your feet all the way through to your hips and lower back, which is exactly what you’ll need as you become more active.
Having OA means managing your symptoms for the rest of your life. That’s why it’s so important to stay as active as you possibly can for as long as you can. Too many people stay sedentary and let their pain get so out of hand that it becomes too hard to even move. You start facing some real serious health conditions when you get to that point, like diabetes, heart disease, and cancer. Don’t let things get that far. Your physical therapist is there to help you find the right combination of exercises and other kinds of treatment that’ll let you keep living your best life.
Hip Bursitis
The last injury we’ll go over is hip bursitis. There’s a fluid filled sac inside your hip joint called a bursa, which acts as a cushion between your bones. Think of it as bubble wrap, protecting your hip but still letting everything move freely. So, if you have hip bursitis, then your bursa is inflamed and irritated.

Symptoms
Hip bursitis is generally pretty painful, especially in and around your joint. It’s even worse when you’re being active and moving around. Swelling is also common, which makes sense since this is a condition that involves inflammation.
With the swelling usually comes a loss in your range of motion. Your bursa fills the space in your hip joint between the bones, muscles, and tendons. So when it’s inflamed and swollen, it puts extra pressure on everything and there’s less space for your hip to move properly.
Now, if your bursitis is caused by an infection, then you might have some different symptoms. Like with most infections, you may notice your skin discolored or red. If that’s the case, then don’t be surprised if there’s a feeling of warmth radiating from that redness. You may also have the classic fever and chills that come with an infection as well.
Causes
Anyone can develop hip bursitis. In some cases, you can get it after a surgery or from an infection. It can also be caused by certain health conditions like lupus, diabetes, or rheumatoid arthritis.
The most common cause of hip bursitis is repetitive stress or overuse. Whether it’s for your job or just a hobby, spending time in certain positions can put excessive pressure on your hip joint. After a while, all that pressure adds up and causes your bursa to become inflamed.
You might not realize some of the positions or activities you do often actually lead to bursitis. Anything that’s fairly rigorous, like lifting heavy boxes or shoveling snow, probably seems pretty obvious when you think about it. But the risky ones, like gardening, painting, and playing an instrument, are the ones that sneak up on you.
Bursitis can also be the result of trauma. Injuries that directly damage your hip joint, like from a collision while playing sports or a car accident, can cause your bursa to swell. People with physically demanding jobs are more likely to experience traumatic injuries too.
Diagnosing
Diagnosing hip bursitis will start with a physical examination. Your doctor will want to know the type of symptoms you’re experiencing, when they began, and most importantly, if your job or hobby requires any repetitive motions.
From there, the doctor will take a look at your hip and the area around it. They’ll look for signs of swelling and test for any limitations in your range of motion. They may also decide to do some other testing as well. X-rays, MRI’s, and blood panels can be used to rule out similar conditions, it’ll just depend on your symptoms and what the doctor finds.
Treatment
When you get bursitis in your hip, the first thing you’ll want to do is avoid whatever position or activity that’s irritating the bursa. It’s important to give your hip a break from that constant pressure so it can actually heal.
As for treatment, it’ll consist of 2 main things: strengthening your hip and learning how to move in ways that don’t stress the joint. Luckily, both of these can be addressed with physical therapy.
At PT, your therapist will ease into exercises that target the muscles that support your hip and lower back. They’ll also help with your range of motion as well. These exercises can even be done at home on the days you don’t have therapy so you can continue progressing outside of the clinic.
Activity Modification
Things get a bit trickier when risky repetitive movements are a part of your normal day (and are what caused your bursitis in the first place.) If that’s the case, then you’ll need to work on proper posture and techniques to prevent putting too much pressure on your hips. You may have to do things like modifying the way you sit or using a stool to kneel on. Your physical therapist will help you navigate daily living without risking making your injury worse.
Most people start to feel relief within the first few weeks of starting PT. But, the longer you stress the bursa in your hip though, the longer it’ll take for you to recover. Plus, you’re more likely to develop chronic bursitis this way too. Chronic bursitis is when you have repeated episodes of bursitis in the same area. And while hip bursitis can come and go, if you keep doing the same movements or activities that you used to do, it can trigger another episode. That’s why it’s so important to start PT as soon as possible.
Click here to learn more about how Borja Physical Therapy can help treat your hip injury.